Mastering the Role: Tips for Being an Effective Standardized Patient
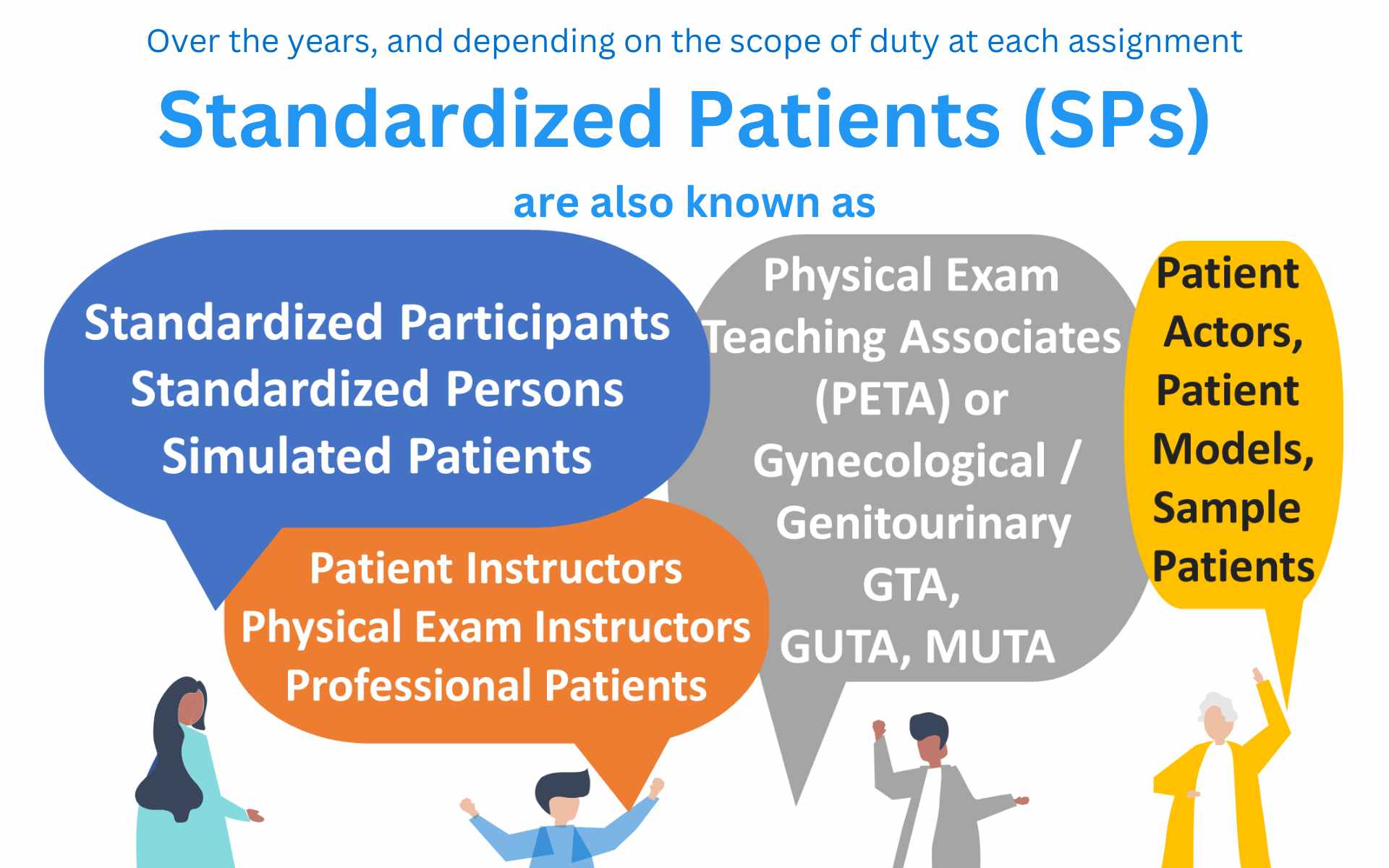
In the world of medical education, standardized patients (SPs) play a vital role in shaping the next generation of healthcare professionals. As the bridge between classroom learning and real-world patient interactions, becoming an effective standardized patient requires more than just memorizing symptoms. In this blog post, we'll look into the importance role that SP plays and delve into the key strategies that can help you excel in this impactful role, making a significant contribution to the development of clinical skills and communication abilities in future doctors.
The Importance of Standardized Patients in Healthcare
In the dynamic landscape of medical education, standardized
patients have emerged as invaluable assets, serving as a bridge between
theoretical learning and real-world patient interactions. Their role extends
far beyond scripted scenarios; they contribute significantly to shaping
competent, empathetic, and patient-centric healthcare professionals. The
importance of standardized patients in healthcare education is rooted in their
ability to provide experiential learning that enhances clinical skills,
communication abilities, and cultural competence.
The concept of using standardized patients in medical education dates back to the mid-20th century. In the 1960s, the introduction of Objective Structured Clinical Examinations (OSCEs) marked a turning point. OSCEs integrated standardized patients into assessments, allowing medical students to demonstrate their clinical and communication skills in controlled settings. Over time, the value of standardized patients became evident, leading to their incorporation into various stages of medical training.
Enhancing Clinical Skills
Standardized patients offer medical learners the opportunity to practice and refine clinical skills without the pressures and complexities of real patient encounters. Students can hone skills such as history-taking, physical examination, and diagnosis, all while receiving immediate feedback. This hands-on experience builds confidence, ensuring that future healthcare professionals are well-prepared to address diverse medical situations competently.
Developing Effective Communication
Effective communication is at the heart of patient-centered
care. Standardized patients enable medical students to practice compassionate
and clear communication, bridging the gap between medical jargon and patient
understanding. Learners gain insights into conveying diagnoses, treatment
plans, and medical information in an empathetic and comprehensible manner.
Cultural Competence and Diversity
In an increasingly diverse healthcare landscape,
standardized patients help students develop cultural competence. By portraying
patients from various backgrounds, they expose learners to different
perspectives, beliefs, and preferences. This exposure fosters cultural
sensitivity, encouraging healthcare providers to offer tailored care that
respects patients' values and needs.
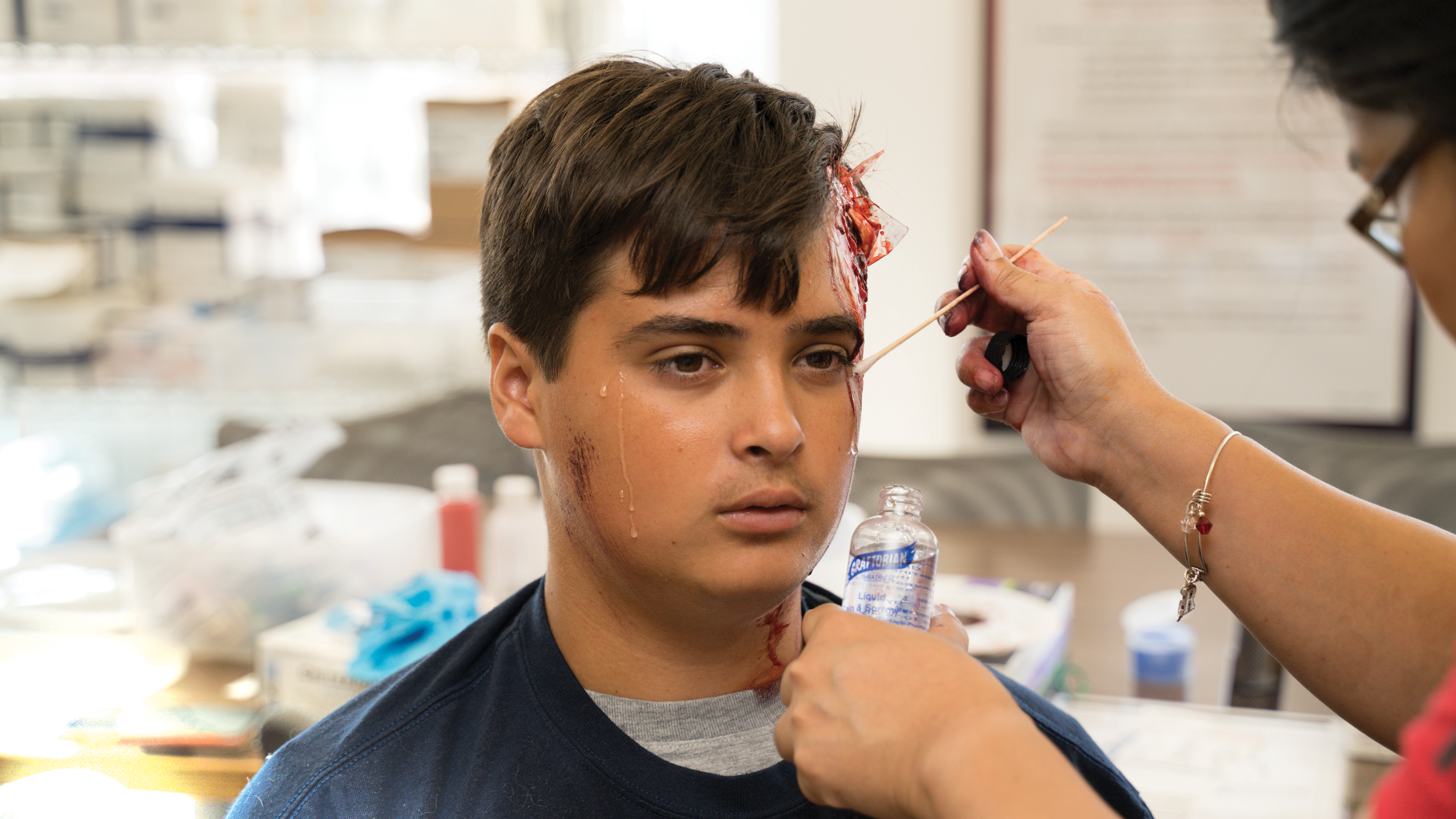
Realism and Safe Learning Environment
Standardized patients introduce realism to medical
education. Learners can practice patient interactions that closely resemble
actual clinical encounters. Mistakes made during simulations offer valuable
learning opportunities without risking patient well-being. This safe
environment encourages experimentation, reflection, and continuous improvement.
Feedback and Self-Reflection
Standardized patients provide immediate feedback to learners, highlighting strengths and areas for improvement. This constructive feedback allows medical students to assess their performance objectively and make necessary adjustments. The process fosters self-awareness and a commitment to ongoing professional development.
Preparation for Complex Cases
Standardized patients can simulate complex medical conditions that medical students might not encounter frequently during their training. This exposure prepares learners for handling a wide range of cases, ensuring they are well-equipped to navigate complex patient histories and diagnostic challenges.
Tips for Portraying as an Standardized Patient
Here are some tips on how to be an effective SP.
1. Understand the Purpose
Before stepping into the role, take the time to understand
the purpose of each simulation. Whether it's helping medical learners practice
diagnosis, communication, or empathy, knowing the educational goals will guide
your portrayal and feedback.
Every scenario calls for a deep dive into research. From
symptoms and medical history to emotional responses, the more you understand,
the more realistic your portrayal will be. Think of yourself as an actor
studying a script, except your performance has real educational value.
3. Consistency and Reliability
Consistency is key to providing a uniform learning
experience for medical students. Strive to maintain the same portrayal across
multiple sessions. Being reliable in attendance and sticking to the script
helps build a consistent and reliable educational environment.
4. Effective Communication
As a standardized patient, your communication skills can impact the realism of the scenario. Use clear language, appropriate tone, and non-verbal cues to engage in a believable patient-doctor interaction.
5. Realistic Emotion Portrayal
Certain scenarios require the portrayal of emotions. Drawing
from personal experiences while keeping a professional distance can add
authenticity to the encounter. Mastering emotional nuances contributes to a
rich learning experience.
6. Giving Constructive Feedback
Your role extends beyond the simulation itself. Effective
feedback can guide medical learners toward improvement. Be specific, highlight
strengths, and provide suggestions for areas that need enhancement.
7. Cultural Sensitivity and Diversity
In a diverse healthcare landscape, cultural sensitivity
matters. Portraying patients from different backgrounds authentically can help
medical students develop cultural competence, enhancing their ability to
provide patient-centered care.
8. Maintaining Patient Confidentiality
Confidentiality is a cornerstone of healthcare. Even in a
simulated environment, respecting patient privacy and ethical considerations is
essential. Upholding confidentiality underscores the professionalism of the
role.
9. Flexibility and Adaptability
Adapting to various scenarios is part of the standardized
patient's expertise. Transitioning seamlessly between different roles and
medical conditions contributes to a well-rounded educational experience.
10. Self-Care and Emotional Resilience
Some scenarios can be emotionally challenging. Prioritize
self-care, set emotional boundaries, and seek support when needed. Emotional
resilience ensures your own well-being while delivering effective simulations.
11. Continuous Improvement
Like any skill, being a standardized patient can be continuously refined. Embrace feedback from educators and fellow standardized patients. This dedication to improvement enhances your performance over time.
Conclusion
Becoming an effective standardized patient is not just about
playing a role; it's about shaping the future of healthcare through education.
By mastering these tips, you can contribute significantly to the growth of
medical students and professionals, enriching their clinical skills and
fostering patient-centered care.
References
Cohen, E. R., Barsuk, J. H., Moazed, F., Caprio, T.,
Didwania, A., & McGaghie, W. C. (2009). Making July safer: simulation-based
mastery learning during intern boot camp. Academic Medicine, 84(7), 885-895.
Bokken, L., Rethans, J. J., Scherpbier, A. J., van der
Vleuten, C. P., & Kuijpers, H. J. (2009). Strengths and weaknesses of
simulated and real patients in the teaching of skills to medical students: a
review. Simulation in healthcare, 4(3), 161-169.
Peters, M., Ten Cate, O., & Bedwell, W. L. (2019).
Twelve tips for the implementation of EPAs for assessment and entrustment
decisions. Medical teacher, 41(6), 641-646.
Ponzer, S., Hylin, U., Kusoffsky, A., Lauffs, M., Lonka, K.,
Mattiasson, A. C., ... & Nordström, G. (2013). Teaching emergency medical
skills using computer-based simulation technology: impact on quality of CPR and
motivation. Resuscitation, 84(7), 992-997.
Wilkinson, S., & Page, L. (2011). Why do we use
simulation for learning in the healthcare professions? British Journal of
Anaesthesia, 106(1), 1-4.
Bridges, D. R., Davidson, R. A., Odegard, P. S., Maki, I. V., & Tomkowiak, J. (2011). Interprofessional collaboration: three best practice models of interprofessional education. Medical education online, 16(1), 6035.













Comments
Post a Comment