Understanding Varicose Veins: Causes, Symptoms, and Treatment Options
Varicose veins are a common vascular condition that affects
millions of people worldwide, particularly as they age. These swollen and
twisted veins, often seen in the legs, can be more than just a cosmetic
concern. Understanding varicose veins, their causes, and how to prevent and
manage them is crucial for maintaining leg health and overall well-being.
Understanding Varicose Veins
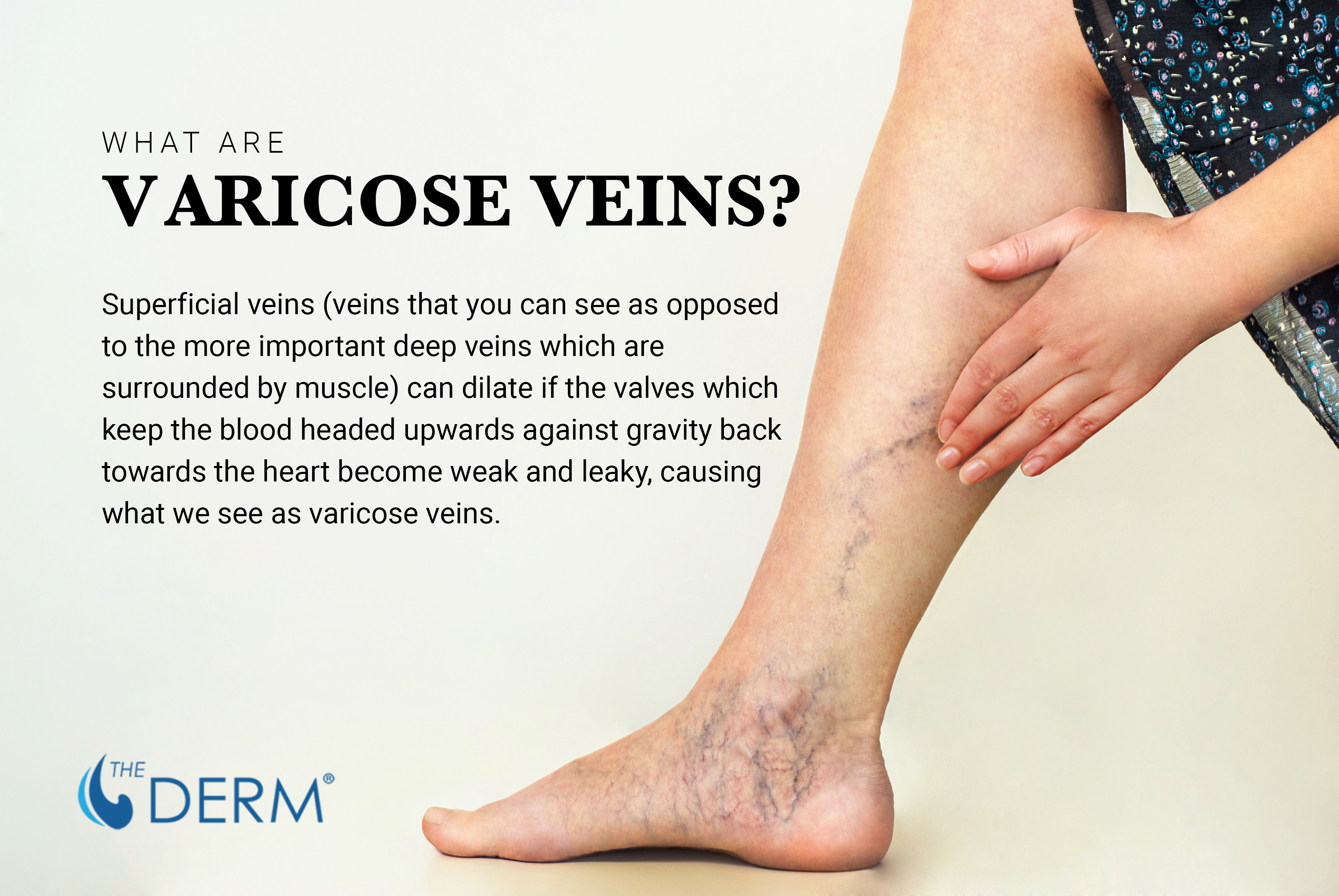
What Are Varicose Veins?
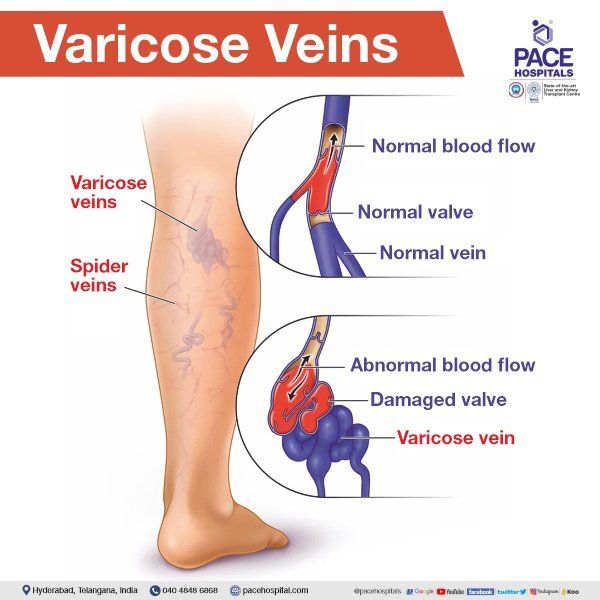
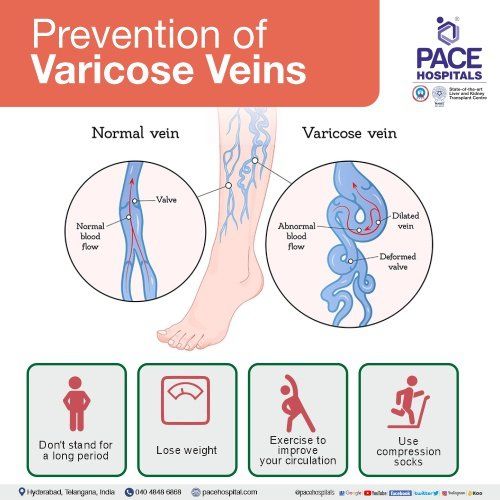
Varicose veins are enlarged, twisted veins that result from damaged or weakened valves within the veins. Varicose veins are a common vascular condition characterized by the enlargement and twisting of veins, typically in the legs.
These veins, which appear as swollen and often blue or purple in color, develop when the blood flow in the veins becomes compromised. Veins have one-way valves that help blood flow upward to the heart. When these valves weaken, blood can pool in the veins, causing them to enlarge and become varicose.
Types of Varicose Veins
Great Saphenous Veins: These are the longest veins in the
body, running along the inner thigh and calf. Varicosities in the great
saphenous veins are often seen as large, rope-like bulges under the skin.
Small Saphenous Veins: These veins are located on the back
of the calf and are responsible for draining blood from the outer calf and
foot. Small saphenous varicose veins may appear as smaller, twisted veins.
Reticular Veins: Reticular veins are smaller, bluish veins
that often appear in clusters just under the surface of the skin. They are
typically less prominent than varicose veins but may contribute to cosmetic
concerns.
Spider Veins (Telangiectasia): Spider veins are tiny, web-like veins that can appear anywhere on the body but are most commonly found on the legs and face. They are often red or blue and may create a spiderweb-like pattern.
Twisting and Enlargement: Varicose veins are characterized
by their twisted and bulging appearance. They can vary in size from small,
superficial veins to larger, more prominent ones.
Color: Varicose veins typically appear blue or purple due to
the pooling of deoxygenated blood within the vein. The color is more noticeable
in larger varicose veins.
Location: Varicose veins are most commonly found in the
legs, especially in areas where veins are under increased pressure, such as the
thighs, calves, and ankles.
Symptoms: Individuals with varicose veins may experience
symptoms such as aching, heaviness, or discomfort in the affected area. These
symptoms often worsen with prolonged standing or sitting.
It's important to note that varicose veins can vary in
severity, from small cosmetic concerns to larger veins that cause discomfort
and require medical attention. Recognizing the type and characteristics of
varicose veins can help individuals seek appropriate treatment and management
options.
In the next sections, we will explore the signs and symptoms
of varicose veins and discuss strategies for prevention and management.
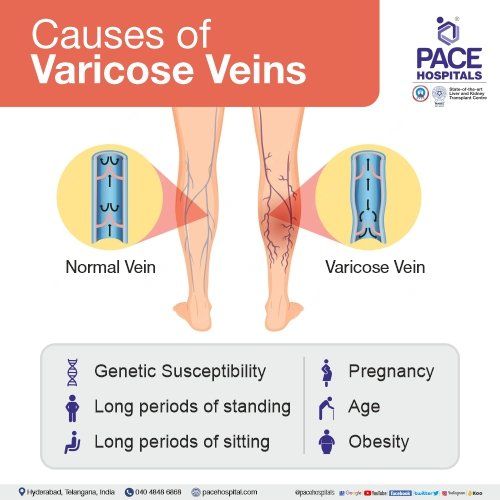
Causes of Varicose Veins
The exact cause of varicose veins can vary, but several
factors contribute to their development:
Genetics: A family history of varicose veins increases the
risk.
Age: The risk increases with age as vein walls weaken.
Gender: Women are more likely to develop varicose veins.
Prolonged Standing or Sitting: Occupations that involve long
periods of standing or sitting can contribute.
Pregnancy: Pregnancy places additional pressure on leg
veins.
Obesity: Excess weight can strain veins and worsen valve
function.
While varicose veins are often considered a cosmetic
concern, they are a clear indication of underlying venous insufficiency and are
associated with various symptoms such as leg pain, aching, and swelling. If
left untreated, varicose veins can progress and contribute to the development
of more severe manifestations of Chronic Venous Disease (CVD), such as venous
ulcers and skin changes.
Chronic Venous Disease (CVD) is a broader vascular condition
that includes a range of venous disorders, with varicose veins being one of its
most common manifestations. CVD encompasses various venous conditions that
involve impaired blood flow in the veins of the legs. Other venous conditions
include:
Venous Ulcers: These are open sores that typically form on
the lower legs due to long-standing venous insufficiency. They can be painful
and challenging to heal.
Venous Eczema (Stasis Dermatitis): This is a skin condition
that results from blood pooling in the veins. It can cause redness, itching,
and inflammation in the lower legs.
Deep Vein Thrombosis (DVT): While DVT is distinct from
varicose veins, it is a significant complication of CVD. DVT is the formation
of blood clots in the deep veins, often in the legs. These clots can be
dangerous if they break free and travel to the lungs (pulmonary embolism).
Signs and Symptoms
Varicose veins often manifest with the following signs and
symptoms:
- Visible, twisted, or bulging veins.
- Aching or throbbing pain in the legs.
- Heaviness or discomfort in the affected area.
- Itchy or irritated skin over the veins.
- Swelling or cramps in the lower legs.
Prevention
Tips for Preventing Varicose Veins
Stay Active: Regular exercise, especially activities that
work the calf muscles, helps improve blood flow in the legs.
Maintain a Healthy Weight: Excess weight places additional
pressure on leg veins.
Elevate Your Legs: Elevating your legs when resting can help
blood flow back to the heart.
Avoid Prolonged Sitting or Standing: Take breaks and change
positions frequently.
Wear Compression Stockings: These provide support to leg
veins and can ease symptoms.
Stay Hydrated: Proper hydration helps maintain healthy blood flow.
Managing Varicose Veins
Non-Invasive Treatments
Non-invasive treatments for varicose veins are typically the
first line of intervention, especially when symptoms are mild to moderate.
These treatments are designed to alleviate discomfort, reduce the appearance of
varicose veins, and improve blood circulation without the need for surgery.
Here are some common non-invasive treatment options.
Compression Stockings: Compression stockings are specially designed elastic stockings that provide gentle pressure on the legs. They work by helping the veins and leg muscles move blood more efficiently. The pressure is greatest at the ankle and gradually decreases as it moves up the leg.
This gradient compression helps prevent blood from pooling in the veins and can significantly reduce symptoms such as aching, swelling, and fatigue. Compression stockings are available in various strengths, and a healthcare professional can recommend the appropriate level of compression.
Research has shown that compression stockings can
effectively reduce leg pain and discomfort associated with varicose veins
[1].
Lifestyle Modifications: Making certain lifestyle changes
can help manage varicose veins and reduce the risk of complications. These
modifications may include:
Regular Exercise: Engaging in low-impact exercises, such as
walking or swimming, can promote better blood circulation in the legs. Leg
muscles act as pumps, helping blood flow back to the heart
Elevating the Legs: Elevating the legs when resting can aid
in reducing swelling and improving blood flow.
Weight Management: Maintaining a healthy weight can reduce
the pressure on leg veins.
Avoiding Prolonged Sitting or Standing: Taking breaks to
move around and avoid prolonged periods of sitting or standing can prevent
blood from pooling in the veins.
Dietary Supplements: Some dietary supplements, such as horse
chestnut seed extract and diosmin, have been studied for their potential
benefits in managing varicose veins. These supplements may help strengthen
blood vessel walls and reduce inflammation. However, it's essential to consult
with a healthcare provider before starting any dietary supplement regimen, as
they can interact with other medications or medical conditions.
Topical Creams and Gels: Over-the-counter or prescription
topical creams and gels may be recommended to relieve symptoms like pain and
itching associated with varicose veins. These products often contain
ingredients such as horse chestnut extract, witch hazel, or aloe vera, which
can provide temporary relief.
Non-invasive treatments are generally well-tolerated and can
effectively manage mild to moderate varicose veins. However, it's important to
note that they may not eliminate varicose veins entirely. If symptoms persist
or worsen despite non-invasive treatments, or if cosmetic concerns remain,
individuals should consult with a healthcare provider to explore other
treatment options, including minimally invasive procedures.
Medical Interventions
In cases where non-invasive methods are insufficient,
medical procedures may be recommended. Endovenous laser therapy (EVLT) and
radiofrequency closure are minimally invasive techniques with high success
rates [2]. These procedures are
designed to address the underlying causes of varicose veins and offer long-term
relief from both symptoms and cosmetic concerns. Here are some of the most
common minimally invasive techniques for varicose vein treatment.
Endovenous Laser Therapy (EVLT): Endovenous laser therapy is
a minimally invasive procedure that uses laser energy to treat varicose veins.
During the procedure, a thin laser fiber is inserted into the affected vein
through a small incision. The laser energy heats and seals the vein, causing it
to collapse and gradually be absorbed by the body. EVLT is highly effective in
treating larger varicose veins and typically requires minimal downtime.
Research has shown that EVLT is a safe and efficient method for treating varicose veins, with high success rates in symptom relief and vein closure [1].
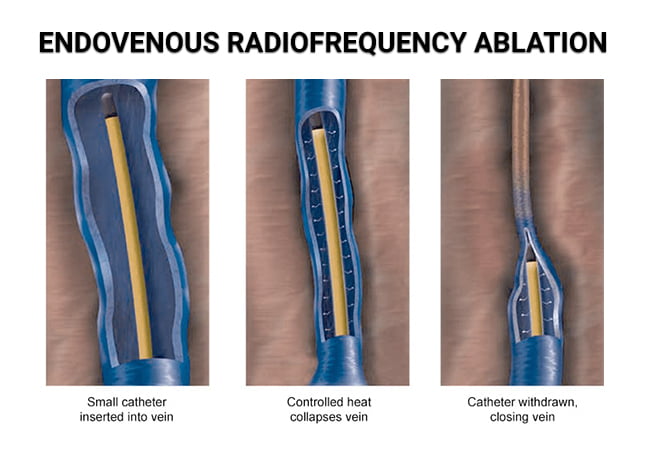
Radiofrequency Ablation (RFA): Radiofrequency ablation is
another minimally invasive technique that uses heat energy to treat varicose
veins. A catheter with a radiofrequency electrode is inserted into the affected
vein, and the heat generated by the electrode causes the vein to close. RFA is
often used for larger veins and has a lower risk of complications compared to
surgical procedures.
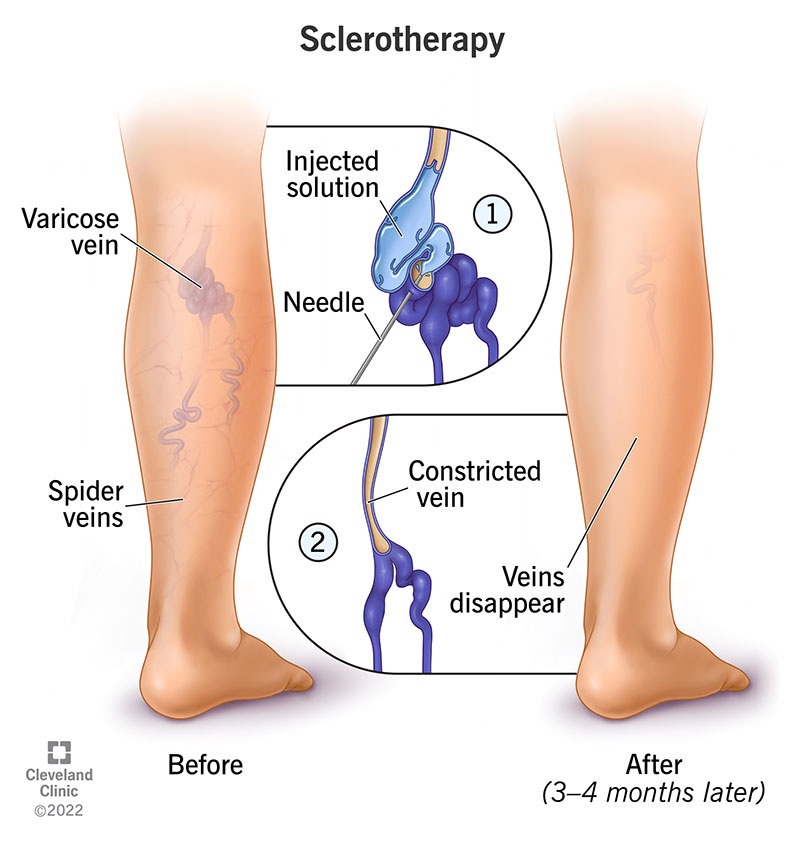
Sclerotherapy: Sclerotherapy is a minimally invasive procedure used to treat smaller varicose veins and spider veins. A special solution, known as a sclerosant, is injected directly into the affected vein. This solution irritates the vein walls, causing them to stick together and eventually close off. Over time, the closed vein is absorbed by the body, and blood flow is redirected to healthier veins.
Sclerotherapy is a well-established and highly effective treatment for smaller varicose veins and spider veins, with minimal discomfort and rapid recovery [^2^].
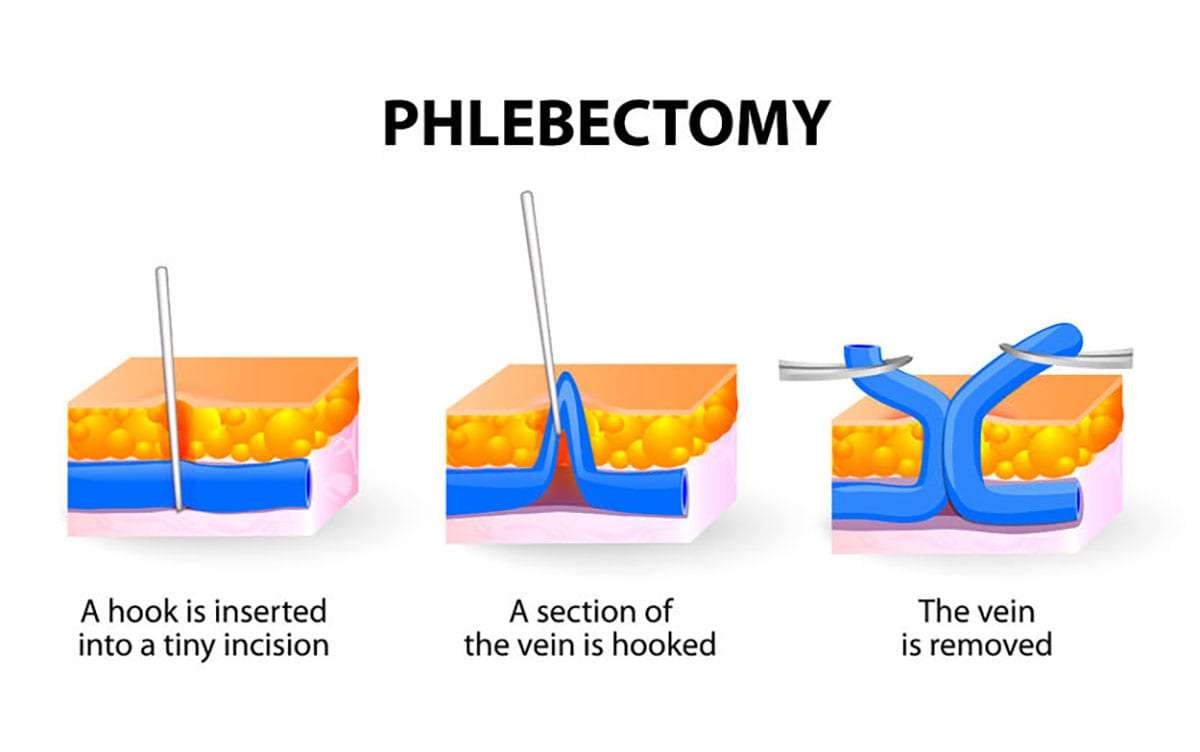
Microphlebectomy: Microphlebectomy, also known as ambulatory phlebectomy, is a procedure used to remove larger surface varicose veins through tiny incisions. A special hook-like instrument is used to gently extract the affected veins.
Microphlebectomy is a minimally invasive technique that results in minimal scarring and is often performed as an outpatient procedure.
Minimally invasive techniques have revolutionized the treatment of varicose veins, offering effective solutions with reduced pain and downtime compared to traditional surgical methods. However, the choice of treatment depends on the size and location of the varicose veins, as well as the individual's overall health and preferences.
Before undergoing any minimally invasive procedure,
individuals should consult with a vascular specialist who can assess their
condition and recommend the most appropriate treatment option based on their
specific needs.
Lifestyle and Home Remedies
In addition to the prevention strategies mentioned earlier,
consider these lifestyle adjustments:
Diet: Consume a diet rich in fiber and antioxidants to
support vein health.
Avoid High Heels: High heels can restrict blood flow in the legs; opt for comfortable footwear.
Leg Exercises: Regularly flex and point your feet to stimulate calf muscles.
When to Seek Medical Help
It's crucial to recognize when medical evaluation is
necessary:
- If you experience pain, swelling, or skin changes in the affected area.
- If varicose veins interfere with your daily activities.
- If you develop leg ulcers or notice bleeding from varicose veins.
Conclusion
Varicose veins are a common condition, but with knowledge
and proactive measures, their impact can be minimized. Understanding the
causes, recognizing symptoms, and implementing prevention strategies are key
steps in managing varicose veins effectively. Seeking medical advice when
needed ensures that you receive the appropriate care and can maintain leg
health for years to come.
Remember, while varicose veins may be common, they are
treatable, and early intervention can prevent complications. Take proactive
steps to care for your leg health, and consult with a healthcare professional
for personalized guidance.
References:
Rabe, E. et al. (2016). Indications for medical compression
stockings in venous and lymphatic disorders: An evidence-based consensus
statement. Phlebology, 31(1_suppl), 1-7.
Almeida, J. I. et al. (2011). Radiofrequency endovenous
ClosureFAST versus laser ablation for the treatment of great saphenous reflux:
a multicenter, single-blinded, randomized study (RECOVERY study). Journal of
Vascular and Interventional Radiology, 22(6), 735-743.








Comments
Post a Comment