Understanding Metabolic Syndrome: Risk Factors, Effects, and Prevention
Metabolic syndrome is a cluster of conditions that, when occurring together, significantly increase the risk of serious health issues. It's a term used to describe a combination of factors that contribute to heart disease, stroke, and type 2 diabetes. This condition is of growing concern worldwide due to its high prevalence and its association with obesity and sedentary lifestyles. In this article, we'll delve into the details of metabolic syndrome, its risk factors, health effects, and most importantly, strategies for prevention and management.
Prevalence
of Metabolic Syndrome
Metabolic syndrome is a global health challenge that affects millions of individuals. According to recent studies, the prevalence of metabolic syndrome varies by region, with higher rates observed in Western countries. Globally, it's estimated that around 25-30% of adults have metabolic syndrome.
In Singapore, as in
many developed nations, metabolic syndrome is a growing health concern. While
precise prevalence rates may vary by study, research indicates that a
significant portion of the population is affected. One study found that
approximately 23.5% of Singaporean adults had metabolic syndrome. As the nation
grapples with modern lifestyles and dietary changes, understanding and addressing
metabolic syndrome are crucial steps in promoting public health.
What Is
Metabolic Syndrome?
Metabolic syndrome
is not a single disease but a collection of risk factors that increase the
chances of developing heart disease, stroke, and type 2 diabetes. To be
diagnosed with metabolic syndrome, an individual typically must have three or
more of the following components:
- Excess abdominal fats: These are evident around the waistline.
- High blood pressure: Elevated blood pressure levels.
- High blood sugar: Elevated fasting blood glucose levels.
- High triglycerides: Elevated levels of fats in the blood.
- Low HDL cholesterol: Low levels of "good" cholesterol.
Abdominal
Obesity
Abdominal obesity,
often referred to as central obesity, plays a pivotal role in the development
of metabolic syndrome. It is characterized by an excess accumulation of fat
around the abdominal area, particularly in the visceral adipose tissue—the fat
stored deep within the abdomen around vital organs like the liver, pancreas,
and intestines. Unlike subcutaneous fat, which is located just beneath the
skin, visceral fat is metabolically active and releases inflammatory substances
and hormones that can disrupt the body's normal functioning.
Determining Abdominal Obesity: Waist Circumference and Body Shape
Waist
Circumference: A key way to determine abdominal obesity is by measuring waist
circumference. It provides a straightforward and reliable assessment of excess
abdominal fat. For both men and women, elevated waist circumference is often a
precursor to metabolic syndrome. Specific cutoff points are used to define
abdominal obesity:
In men, a waist
circumference of 40 inches (102 cm) or more is considered indicative of
abdominal obesity.
In women, a waist
circumference of 35 inches (88 cm) or more suggests abdominal obesity.
Another indicator of abdominal obesity is body shape. Individuals with an "apple-shaped" body tend to carry excess fat in the abdominal area, while those with a "pear-shaped" body tend to accumulate fat in the hips and thighs. The apple shape, associated with abdominal obesity, is a significant risk factor for metabolic syndrome.
Abdominal obesity
is not just a cosmetic concern; it has profound implications for metabolic
health. Visceral fat is metabolically active and releases substances like
adipokines and cytokines that promote inflammation and insulin resistance.
These factors contribute to various components of metabolic syndrome, including
high blood pressure, high blood sugar, and abnormal lipid profiles.
In addition to the metabolic risks, abdominal obesity is also linked to an increased risk of cardiovascular disease and a higher likelihood of developing type 2 diabetes.
High Blood
Pressure
High blood pressure, also known as hypertension, is one of the primary components of metabolic syndrome. It's a condition characterized by elevated blood pressure levels, and it significantly contributes to the development of metabolic syndrome.
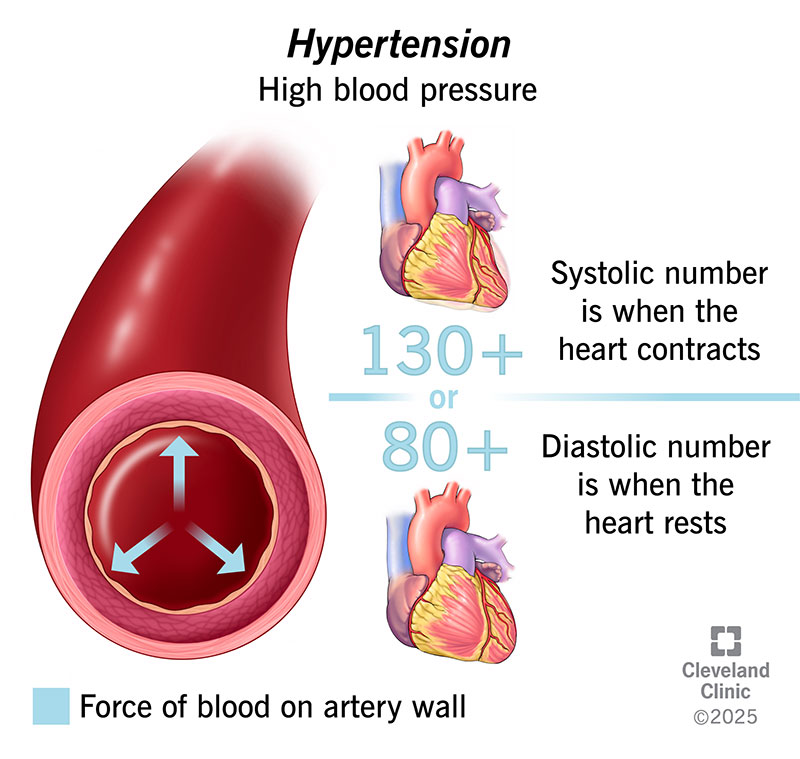
Blood pressure is measured in millimeters of mercury (mm Hg) and is expressed as two values: systolic pressure (the higher number) and diastolic pressure (the lower number).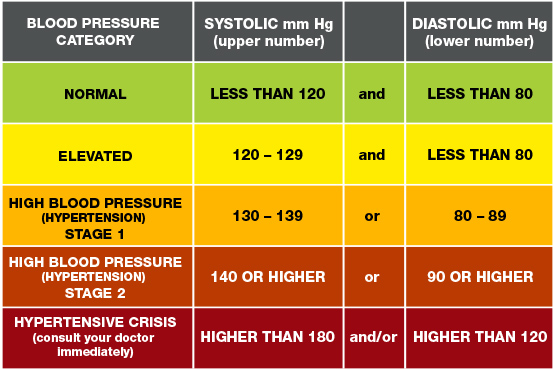
Normal blood pressure is typically considered to be around 120/80 mm Hg. High blood pressure is diagnosed when blood pressure consistently exceeds 130/85 mm Hg or when individuals are already on medication for hypertension. This results in risk of metabolic syndrome as follows:
Insulin Resistance:
High blood pressure and insulin resistance are closely related. Insulin
resistance impairs the body's ability to use glucose effectively, which can
lead to higher insulin levels in the blood. Elevated insulin levels contribute
to sodium retention and an increase in blood pressure.
Inflammation:
Chronic inflammation, often associated with obesity, is a common factor in both
high blood pressure and metabolic syndrome. Inflammatory substances can damage
blood vessel walls, making them less elastic and more resistant to blood flow,
leading to elevated blood pressure.
Atherosclerosis:
Metabolic syndrome components, including high blood pressure, contribute to the
development of atherosclerosis, a condition where arteries become narrowed and
hardened due to the buildup of plaque. Atherosclerosis can further increase
blood pressure.
The health Implications of High Blood Pressure are:
Cardiovascular
Disease: High blood pressure is a significant risk factor for cardiovascular
disease, including heart attacks and strokes. In the context of metabolic
syndrome, the combination of elevated blood pressure with other risk factors
amplifies the risk of heart-related complications.
Organ Damage:
Prolonged high blood pressure can damage blood vessels, the heart, and other
vital organs like the kidneys. This can lead to conditions such as kidney
disease and heart failure.
Worsening Insulin
Resistance: High blood pressure can worsen insulin resistance, creating a
vicious cycle that exacerbates metabolic syndrome components.
High Blood Sugar (Hyperglycemia)
High blood sugar, also known as hyperglycemia, is a fundamental component of metabolic syndrome. It represents elevated levels of glucose (sugar) in the development and progression of this complex condition. Blood sugar levels are typically measured in milligrams per deciliter (mg/dL) and vary throughout the day. Fasting blood sugar levels below 100 mg/dL are considered normal. Levels between 100 mg/dL and 125 mg/dL may indicate prediabetes, while levels of 126 mg/dL or higher on two separate tests generally diagnose diabetes.Insulin Resistance:
One of the key features of metabolic syndrome is insulin resistance, a
condition in which the body's cells do not respond effectively to insulin. This
results in elevated blood sugar levels because glucose cannot enter the cells
properly.
Elevated Insulin
Levels: To compensate for insulin resistance, the pancreas often produces more
insulin. Elevated insulin levels contribute to high blood pressure and an
increased risk of cardiovascular disease, both of which are components of
metabolic syndrome.
Inflammation:
Chronic inflammation, often associated with obesity, can further impair insulin
sensitivity and contribute to high blood sugar levels.
The health Implications of High Blood Sugar are:
Type 2 Diabetes:
Prolonged high blood sugar levels can lead to the development of type 2
diabetes, a condition in which the body cannot regulate blood sugar
effectively. Type 2 diabetes is a hallmark feature of metabolic syndrome.
Cardiovascular
Risk: High blood sugar is a significant risk factor for cardiovascular disease,
including heart attacks and strokes. It intensifies the cardiovascular risks
associated with other metabolic syndrome components.
Complications: Over
time, uncontrolled high blood sugar can lead to various complications,
including kidney disease, nerve damage, vision problems, and poor wound
healing.
High Triglycerides
High triglycerides are a significant component of metabolic syndrome, contributing to the complexity of this condition. Triglycerides are a type of fat found in your blood, and elevated levels can have profound implications for your health. Triglyceride levels are measured in milligrams per deciliter (mg/dL) and are considered normal when they are below 150 mg/dL. Levels between 150 mg/dL and 199 mg/dL are borderline high, and levels of 200 mg/dL or higher are considered high.
The connection to metabolic syndrome includes:
Insulin Resistance:
Like other components of metabolic syndrome, high triglycerides are often
linked to insulin resistance. Insulin resistance can lead to increased
production of triglycerides by the liver.
Excess Calories:
Consuming more calories than the body can burn, especially from sugary and
high-fat foods, can lead to elevated triglyceride levels. This often goes hand
in hand with obesity, another metabolic syndrome component.
Lifestyle Factors: Sedentary lifestyles, excessive alcohol consumption, and smoking are all factors that can contribute to high triglycerides and metabolic syndrome.
High triglycerides raise the risks of :
Cardiovascular disease: Elevated triglycerides are associated with an increased risk of cardiovascular
disease. They can contribute to the buildup of fatty deposits in the arteries,
which can narrow and harden the blood vessels, raising the risk of heart
attacks and strokes.
Pancreatitis:
Extremely high triglyceride levels can lead to pancreatitis, a painful
inflammation of the pancreas.
Metabolic
Abnormalities: High triglycerides often accompany other metabolic
abnormalities, including low HDL cholesterol and insulin resistance, further
complicating the metabolic syndrome picture.
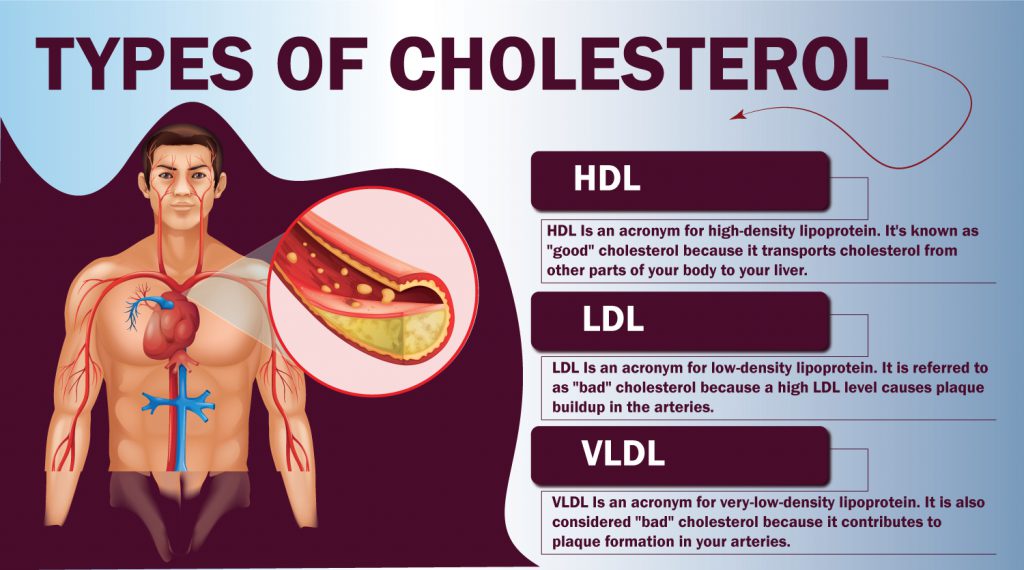
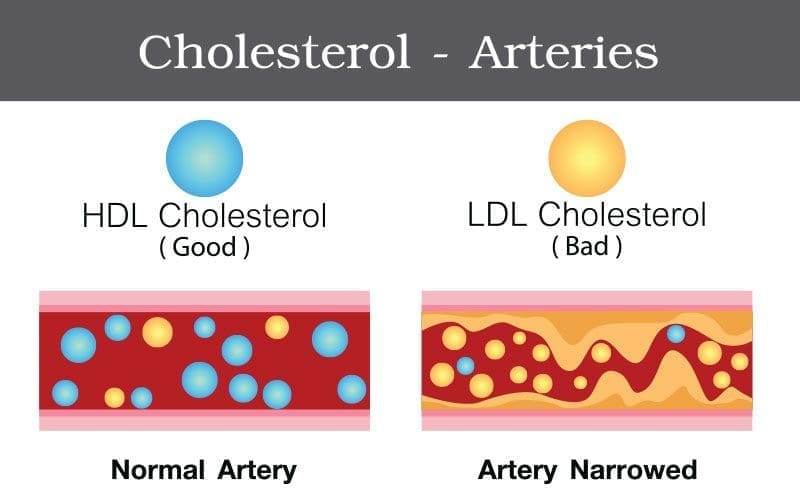
Low HDL Cholesterol
Low high-density lipoprotein (HDL) cholesterol, often referred to as "good" cholesterol, is a vital component of metabolic syndrome. HDL cholesterol is one of the two main types of cholesterol found in your blood, the other being low-density lipoprotein (LDL) cholesterol. HDL cholesterol is often considered "good" because it helps remove excess cholesterol from the bloodstream and transport it to the liver for elimination.
Typically, a higher level of HDL cholesterol is considered desirable for overall health. A level below 40 mg/dL in men and below 50 mg/dL in women is considered low.
HDL cholesterol plays a part in the following:
Reverse Cholesterol
Transport: HDL cholesterol plays a crucial role in reverse cholesterol
transport, a process by which excess cholesterol is removed from cells and
tissues and transported back to the liver. Low HDL levels can hinder this
process, contributing to the accumulation of cholesterol in the blood vessels.
Atherosclerosis:
Low HDL cholesterol is associated with an increased risk of atherosclerosis, a
condition characterized by the buildup of fatty deposits (plaque) in the
arteries. This can narrow the arteries and reduce blood flow, leading to
various cardiovascular issues.
Inflammation: Low
HDL levels are often linked to inflammation, which can further contribute to
atherosclerosis and other metabolic syndrome components.
Low HDL cholesterol can results in:
Cardiovascular
Risk: Low HDL cholesterol is a significant risk factor for cardiovascular
disease. It can increase the risk of heart attacks, strokes, and other vascular
complications.
Metabolic
Abnormalities: Low HDL levels are often associated with other metabolic
abnormalities, including high triglycerides and insulin resistance, further
complicating the metabolic syndrome profile.
Causes of Metabolic Syndrome
Metabolic syndrome
is a complex condition with multiple contributing factors. The development of
metabolic syndrome is often the result of a combination of genetic, lifestyle,
and environmental factors. Here, we delve into the primary causes:
1. Genetics
Family History: A
genetic predisposition to metabolic syndrome can increase the likelihood of
developing the condition. If close relatives have metabolic syndrome, your risk
may be higher.
2. Lifestyle
Factors
Dietary Choices:
Diets high in refined sugars, saturated and trans fats, and low in fiber are
linked to an increased risk of metabolic syndrome. Excessive calorie intake and
a diet low in nutrient-dense foods can lead to obesity and insulin resistance.
Physical
Inactivity: Sedentary lifestyles contribute to weight gain and insulin
resistance. Regular physical activity is essential for maintaining a healthy
metabolism.
Smoking: Smoking is
associated with an increased risk of metabolic syndrome and cardiovascular
disease. It can contribute to insulin resistance and worsen existing metabolic
issues.
3. Obesity
Abdominal Obesity:
As discussed earlier, excess abdominal fat, especially visceral fat, is a central
feature of metabolic syndrome. It promotes inflammation and insulin resistance.
4. Insulin
Resistance
Insulin resistance
is a fundamental aspect of metabolic syndrome. It occurs when the body's cells
do not respond efficiently to insulin, leading to elevated blood sugar levels.
Over time, this can lead to type 2 diabetes.
5. Hormonal
Factors
Conditions such as
polycystic ovary syndrome (PCOS) and hormonal imbalances can increase the risk
of metabolic syndrome, particularly in women.
6. Age and Gender
The risk of
metabolic syndrome tends to increase with age. In women, factors like menopause
can contribute to changes in metabolism and abdominal fat distribution.
7. Environmental
Factors
Stress: Chronic
stress can trigger hormonal changes that affect metabolism and contribute to
metabolic syndrome.
Environmental
Toxins: Some environmental pollutants and toxins may play a role in the
development of metabolic syndrome, although more research is needed in this
area.
8. Sleep Disorders
Conditions like
sleep apnea and inadequate sleep can disrupt hormonal balance and contribute to
metabolic issues.
It's important to
note that while these factors can increase the risk of metabolic syndrome, the
condition is preventable and manageable through lifestyle modifications.
Recognizing and addressing these causes is the first step in reducing the risk
and improving overall health.
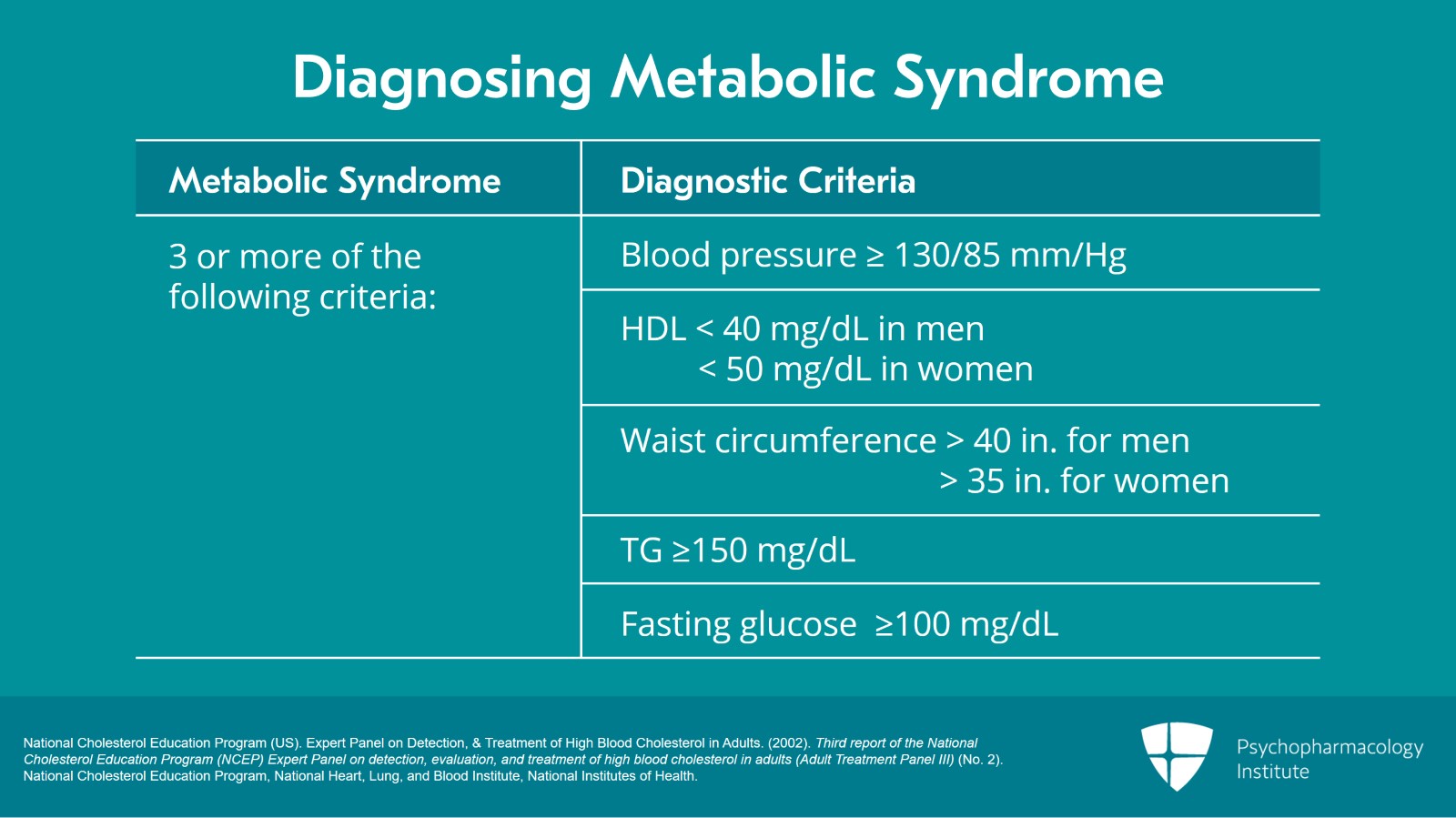
Diagnosing Metabolic Syndrome
Diagnosing
metabolic syndrome involves assessing specific criteria, including waist
circumference, blood pressure, and blood tests for glucose, triglycerides, and
HDL cholesterol levels. Regular health check-ups are important for early
detection and intervention.
Diagnostic
Criteria
Metabolic syndrome
is typically diagnosed when an individual meets three or more of the following
criteria:
Elevated Waist
Circumference: As discussed earlier, an increased waist circumference is a
central feature. Specific cutoff points are used based on gender and
population.
High Blood
Pressure: Blood pressure measurements that exceed 130/85 mm Hg or ongoing
treatment for hypertension meet this criterion.
Elevated Fasting
Blood Sugar: A fasting blood sugar level of 100 mg/dL (5.6 mmol/L) or higher
indicates impaired glucose metabolism or diabetes.
Elevated
Triglycerides: A fasting triglyceride level of 150 mg/dL (1.7 mmol/L) or higher
signifies an abnormal lipid profile.
Low HDL
Cholesterol: HDL cholesterol levels below 40 mg/dL (1.0 mmol/L) for men and
below 50 mg/dL (1.3 mmol/L) for women are considered low.
Diagnostic Tests
To confirm these
criteria, healthcare providers may order the following tests:
Blood Pressure
Measurement: This is a routine measurement to assess if blood pressure levels
are within the specified range.
Fasting Blood Sugar Test: A blood sample is taken after an overnight fast to measure fasting blood glucose levels. Elevated levels suggest impaired glucose metabolism.
Lipid Profile: This blood test measures triglycerides, HDL cholesterol, and LDL cholesterol levels. Abnormal results indicate lipid imbalances.
Waist Circumference Measurement: A tape measure is used to determine waist circumference, focusing on the midpoint between the lower margin of the last rib and the top of the hip bone.
Other Tests: Depending on the individual's medical history and risk factors, additional tests such as HbA1c (glycated hemoglobin) or glucose tolerance tests may be recommended to assess glucose control.
Once diagnosed with metabolic syndrome, ongoing monitoring is essential to track progress and assess the effectiveness of lifestyle changes and treatments. This may include regular blood pressure checks, lipid profiles, and glucose monitoring.
Prevention and
Management
Preventing and
managing metabolic syndrome primarily involves lifestyle changes:
Weight Management:
Achieving and maintaining a healthy weight through diet and exercise is key.
Regular Physical
Activity: Engaging in regular exercise improves insulin sensitivity and overall
metabolic health.
Balanced Diet: A
diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats
can help control blood sugar and cholesterol levels.
Smoking Cessation:
Quitting smoking is essential for reducing cardiovascular risks.
Medications: In
some cases, medications may be prescribed to manage specific components of
metabolic syndrome, such as high blood pressure or high cholesterol.
For individuals diagnosed with metabolic syndrome, it's crucial to:
Follow Medical
Advice: Adherence to prescribed medications and lifestyle recommendations is
essential.
Monitor Health:
Regularly check blood pressure, blood sugar, and cholesterol levels.
Seek Support:
Consider joining support groups or working with a healthcare professional to
address emotional and practical challenges.
Conclusion
In conclusion,
metabolic syndrome is a serious health condition that affects millions of
people worldwide. However, it is preventable and manageable through lifestyle
changes and medical intervention. Awareness, early detection, and proactive
steps toward better metabolic health are key to reducing the risks associated
with this condition.





:max_bytes(150000):strip_icc()/Health-Zoe-Hansen-high-blood-sugar-final-f6dc79d38b4b423ab54c96dad3594207.jpg)





:max_bytes(150000):strip_icc()/understanding-the-fasting-plasma-glucose-test-1087680-ADD-FINAL-B-f9a36a14160b442ab9e829c5ebb81c49.png)
:max_bytes(150000):strip_icc()/697547_color-5ba2929346e0fb0025757b04.png)





Comments
Post a Comment