Depression: Recognizing the Signs and Seeking Help
Depression is not just a passing feeling of sadness; it's a complex and serious mental health condition that affects millions of people worldwide. Despite its prevalence, depression often goes unrecognized and untreated. In this blog post, we'll delve into the world of depression, helping you recognize its signs and understand the importance of seeking help when needed.
Understanding Depression
Depression, also
known as major depressive disorder, is characterized by persistent feelings of
sadness, hopelessness, and a lack of interest or pleasure in daily activities.
It's essential to distinguish clinical depression from ordinary sadness or
grief, as it often requires professional intervention.
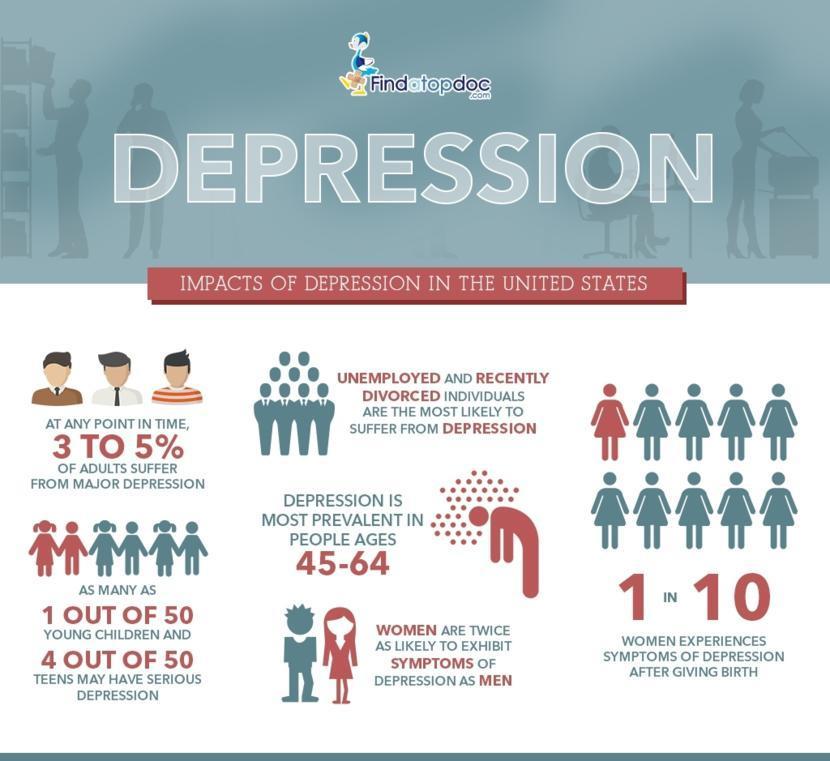
An estimated 3.8% of the population experience depression, including 5% of adults (4% among men and 6% among women), and 5.7% of adults older than 60 years. Approximately 280 million people in the world have depression (1). Depression is about 50% more common among women than among men. Worldwide, more than 10% of pregnant women and women who have just given birth experience depression (2). More than 700 000 people die due to suicide every year. Suicide is the fourth leading cause of death in 15–29-year-olds.
Singapore conducts regular mental health surveys to assess the prevalence of various mental health conditions, including depression. According to the Singapore Mental Health Study 2018, about 1 in 16 people in Singapore (6.3% of the population) experienced a mood disorder like major depressive disorder or bipolar disorder at some point in their lives.
There are various
types of depression, each with its unique features. Major depressive disorder
is the most common, while persistent depressive disorder involves long-lasting
symptoms. Here are some of the key types of depression as per Diagnostic and
Statistical Manual of Mental Disorders, Fifth Edition (DSM-5):
1. Major Depressive
Disorder (MDD)
MDD, often referred
to as clinical depression, is characterized by persistent feelings of sadness,
loss of interest or pleasure in activities, and a range of other emotional and
physical symptoms.
To meet the
criteria for MDD, a person must experience five or more of these symptoms
during the same two-week period. These symptoms include changes in appetite or
weight, sleep disturbances, fatigue, feelings of worthlessness or guilt,
difficulty concentrating, and thoughts of death or suicide.
Major depressive
episodes can occur multiple times in a person's life.
2. Persistent
Depressive Disorder (Dysthymia)
Persistent
depressive disorder, also known as dysthymia, is characterized by a chronic,
low-level depression lasting for at least two years in adults (or one year in
children and adolescents).
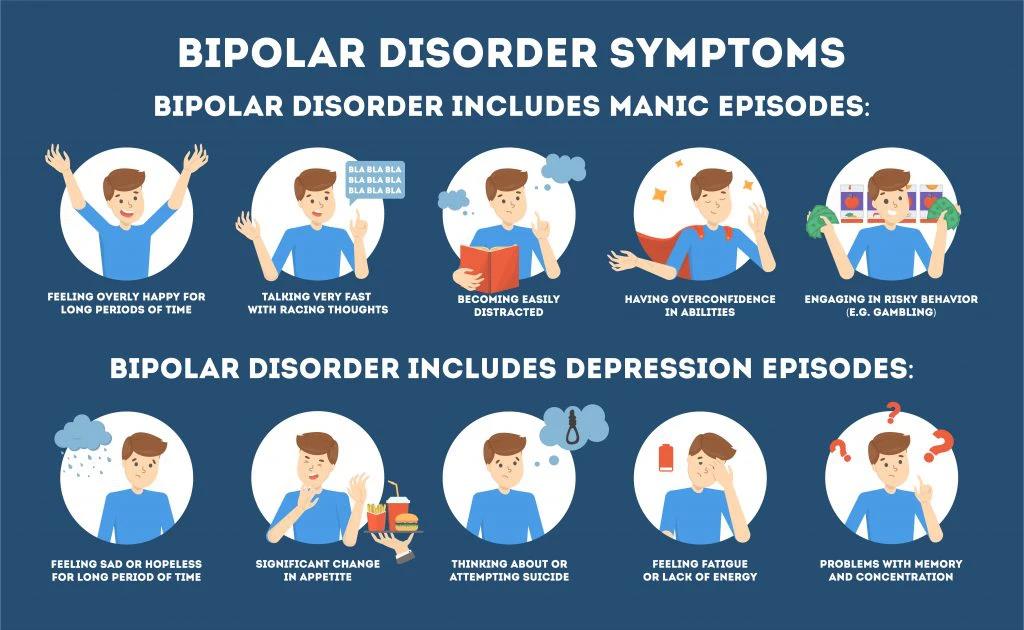
3. Bipolar Disorder
(formerly known as Manic-Depressive Illness)
Bipolar disorder involves cycling between periods of depression and periods of mania or hypomania (less severe than mania). There are several types of bipolar disorder, including bipolar I and bipolar II.
4. Seasonal
Affective Disorder (SAD)
SAD is a type of
depression that follows a seasonal pattern, with symptoms typically occurring
during the fall and winter months when there is less natural sunlight. Common
symptoms include sadness, changes in appetite and sleep patterns, weight gain,
and a lack of energy.
Here are some of the key factors:
Biological Factors
Genetics: There is
evidence that genetic factors play a role in depression. People with a family
history of depression may be more predisposed to the condition.
Neurochemistry:
Imbalances in neurotransmitters like serotonin, norepinephrine, and dopamine
are associated with depression. Medications like antidepressants often target
these imbalances.
Brain Structure and
Function
Changes in the
brain's structure and function can contribute to depression. The hippocampus,
prefrontal cortex, and amygdala are areas of the brain involved in mood
regulation, and alterations in these regions have been observed in people with
depression.
Hormonal Changes
Hormonal fluctuations can influence mood. For example, hormonal changes during pregnancy, postpartum, and menopause can increase the risk of depression in women. Thyroid disorders and hormonal imbalances can also contribute to depressive symptoms.
Environmental
Factors
Stress: Chronic
stress can increase the risk of depression. Prolonged exposure to stress
hormones like cortisol may affect brain function and mood regulation.
Trauma:
Experiencing trauma, such as physical, emotional, or sexual abuse, can increase
the risk of depression later in life.
Early Life
Experiences: Adverse childhood experiences, neglect, or exposure to a
dysfunctional family environment can contribute to depression in adulthood.
Medical Conditions
Certain medical conditions, such as chronic illnesses (e.g., cancer, diabetes), chronic pain, and neurological disorders, can increase the risk of depression. Medications used to treat these conditions may also have depressive side effects.
Substance Abuse
Substance abuse,
including alcohol and drug misuse, can contribute to or exacerbate depression.
Substance use can temporarily alleviate symptoms but often worsens the
condition in the long run.
Personality and
Psychological Factors
Certain personality traits, such as high levels of neuroticism or perfectionism, may increase susceptibility to depression. Negative thinking patterns, low self-esteem, and a history of past episodes of depression can also be risk factors.
Social and
Environmental Factors
Socioeconomic status, access to healthcare, and social support systems can influence the risk of depression. Loneliness, isolation, and a lack of a strong support network can contribute to depressive symptoms.
Life Events
Major life events,
such as the loss of a loved one, divorce, job loss, or financial stressors, can
trigger depressive episodes, especially in individuals with a vulnerability to
depression.
Cultural and
Societal Factors
Cultural norms and
societal expectations regarding emotions and mental health can affect how
individuals perceive and express depressive symptoms.
It's important to
note that depression is often the result of a combination of these factors, and
not everyone with these risk factors will develop depression. Additionally,
identifying and addressing these contributing factors is an essential part of
depression treatment and prevention. A comprehensive approach that considers
biological, psychological, and environmental factors is often the most
effective way to manage depression.
Recognizing the
Signs
Recognizing the signs of depression is the first step toward seeking help. Depression manifests differently in each individual, but common symptoms include:
Persistent Sadness:
Individuals with depression often experience a deep and pervasive sense of
sadness that lasts for most of the day, nearly every day. This sadness can feel
overwhelming and unshakeable, and it doesn't always have an apparent cause.
Loss of Interest or
Pleasure: A hallmark of depression is anhedonia, or the inability to find joy
or pleasure in activities or hobbies that were once enjoyable. Individuals may
lose interest in things they used to love and may withdraw from social
engagements.
Changes in Appetite
or Weight: Depression can lead to changes in appetite. Some people may
experience a significant increase in appetite and weight gain, while others may
have a reduced appetite and lose weight. These changes are often unrelated to
intentional dieting.
Sleep Disturbances:
Sleep problems are common in depression. Some individuals may struggle with
insomnia, finding it difficult to fall asleep or stay asleep. Others may
experience hypersomnia, where they sleep excessively but still feel fatigued.
Fatigue and Lack of
Energy: Individuals with depression often report persistent feelings of fatigue
and a lack of physical or mental energy. Simple tasks may feel exhausting, and
motivation can be challenging to muster.
Feelings of
Worthlessness or Guilt: Many people with depression have low self-esteem and
may harbor feelings of worthlessness or guilt over perceived failures or
shortcomings. These feelings can be irrational and disproportionate to the
circumstances.
Difficulty
Concentrating: Depression can impair cognitive function, making it hard for individuals
to concentrate, make decisions, or remember things. This "brain fog"
can impact daily functioning.
Psychomotor
Agitation or Retardation: Some individuals with depression experience physical
restlessness or agitation, while others may become noticeably slowed down in
their movements and speech.
Suicidal Thoughts:
In severe cases of depression, individuals may have thoughts of death or
suicide. It's crucial to take any mention of suicidal thoughts seriously and
seek immediate help.
Physical Symptoms:
Depression can manifest physically, leading to headaches, digestive problems,
and unexplained aches and pains. These physical symptoms often occur in
conjunction with emotional distress.
Irritability:
Depression can lead to increased irritability, where even minor frustrations
can trigger intense emotional reactions.
Social Withdrawal:
Individuals with depression may isolate themselves from friends and family,
often because they lack the energy or motivation to engage in social
interactions.
It's important to
remember that not everyone with depression will experience all of these
symptoms, and the severity of symptoms can vary widely from person to person.
Additionally, the presence of these symptoms for an extended period (typically
at least two weeks) is a key diagnostic criterion for major depressive disorder
(MDD). If you or someone you know is experiencing symptoms of depression, it's
essential to seek help from a mental health professional for an accurate
diagnosis and appropriate treatment. Depression is a treatable condition, and
many individuals find relief with therapy, medication, or a combination of
both.
Risk Factors and
Vulnerable Populations
Certain factors
increase the risk of developing depression. Genetics, trauma, chronic stress,
and certain medical conditions can contribute. Some populations, such as
adolescents and older adults, are more vulnerable to depression due to life
transitions and unique challenges. The
risk factors for depression are:
Family History: A
family history of depression or other mood disorders increases the risk of
developing depression. Genetics play a role in susceptibility to the condition.
Personal History:
Individuals who have experienced one or more episodes of depression in the past
are at a higher risk of recurrent depressive episodes.
Trauma and Stress:
Exposure to trauma, such as physical, emotional, or sexual abuse, as well as
significant life stressors like divorce, job loss, or the death of a loved one,
can trigger or exacerbate depression.
Chronic Illness:
People with chronic medical conditions, such as diabetes, heart disease, or
cancer, are at a higher risk of developing depression. The emotional and
physical burden of managing a chronic illness can contribute to depressive
symptoms.
Substance Abuse:
Misuse of alcohol, drugs, or prescription medications can increase the risk of
depression. Substance abuse often co-occurs with depression, and the
relationship between the two is complex.
Medications: Some
medications, such as certain antihypertensives, corticosteroids, and
isotretinoin (used to treat severe acne), have been linked to depressive side
effects.
Hormonal Changes:
Hormonal fluctuations can impact mood. This includes hormonal changes during
pregnancy, postpartum, perimenopause, and menopause in women.
Chronic Pain:
Persistent pain conditions, such as fibromyalgia or arthritis, can contribute
to depression. The experience of chronic pain can erode one's quality of life
and emotional well-being.
Lack of Social
Support: A lack of social connections and support can increase the risk of
depression. Loneliness and isolation can exacerbate depressive symptoms.
Economic
Disadvantage: Socioeconomic factors, including poverty, unemployment, and
financial instability, are associated with a higher risk of depression.
Some population, such as adolescents and older adults, are more vulnerable to depression due to life transitions and unique challenges. These vulnerable population, which encompass various groups defined by age, gender, socioeconomic status, or life circumstances, are often at a higher risk of developing depression due to a combination of unique stressors, challenges, and societal factors. Understanding why these populations are susceptible to depression is essential in addressing the mental health needs of diverse communities and tailoring interventions to offer support where it's needed most.
Children and
Adolescents: Depression can occur at any age, but it often emerges during
adolescence. Academic pressures, peer relationships, and hormonal changes can
contribute to the development of depression in young people.
Women: Women are
more likely than men to experience depression. Hormonal factors, such as those
related to menstruation, pregnancy, postpartum, and menopause, can contribute
to this gender disparity.
Older Adults:
Depression is not a normal part of aging, but older adults may face unique risk
factors, including chronic health conditions, social isolation, and the loss of
loved ones.
LGBTQ+ Individuals:
Members of the LGBTQ+ community may face discrimination, stigma, and social
rejection, which can contribute to higher rates of depression.
Military Veterans:
Military service members and veterans may experience depression related to
combat exposure, traumatic experiences, and the challenges of transitioning to
civilian life.
Chronic Illness
Patients: Individuals with chronic medical conditions, such as cancer,
diabetes, or multiple sclerosis, are at an increased risk of depression due to
the emotional and physical toll of their conditions.
Caregivers: Those
who provide care for individuals with chronic illnesses or cognitive
impairments, such as Alzheimer's disease, can experience caregiver stress and
are at risk of depression.
People with
Substance Use Disorders: Substance use and depression often co-occur. Substance
misuse can contribute to the development and exacerbation of depressive
symptoms.
Minority and
Disadvantaged Communities: Minority populations, particularly those with
limited access to healthcare and facing systemic discrimination, may be at a
higher risk of depression.
It's important to
note that anyone, regardless of age, gender, or background, can experience
depression. Additionally, individuals with depression can recover and manage
their condition with appropriate treatment, support, and coping strategies.
Early intervention is crucial for improving outcomes and reducing the impact of
depression on individuals and their communities.
Diagnosis of
Depression
Diagnosing depression is a crucial step in providing appropriate care and support. Mental health professionals use standardized criteria to assess whether an individual meets the criteria for depression. Diagnosis typically involves the following components:
Clinical
Assessment: Mental health professionals, such as psychiatrists, psychologists,
or licensed therapists, conduct a comprehensive clinical assessment. This
includes gathering information about the individual's symptoms, personal
history, and any potential triggers for their depressive episode.
Diagnostic
Criteria: Depression is diagnosed based on specific criteria outlined in
diagnostic manuals like the Diagnostic and Statistical Manual of Mental
Disorders (DSM-5). These criteria include the presence of specific symptoms
over a certain duration, often lasting at least two weeks, and the impact of
these symptoms on daily functioning.
Psychological Evaluation: Psychological assessments and questionnaires may be administered to evaluate the severity of depressive symptoms and assess potential co-occurring conditions, such as anxiety or bipolar disorder.
Physical Examination:
In some cases, a physical examination and laboratory tests may be conducted to
rule out underlying medical conditions that could be contributing to the
symptoms.
Differential
Diagnosis: The clinician will also consider other conditions that may mimic
depression, such as bipolar disorder, medical illnesses, or substance use
disorders, to ensure an accurate diagnosis.
Patient's Input:
The individual's own description of their symptoms and experiences is vital in
the diagnostic process. Open and honest communication between the patient and
healthcare provider is encouraged.
Once a diagnosis of depression is established, a tailored treatment plan can be developed. The choice of treatment may depend on the severity of symptoms, any co-occurring conditions, and the individual's preferences.
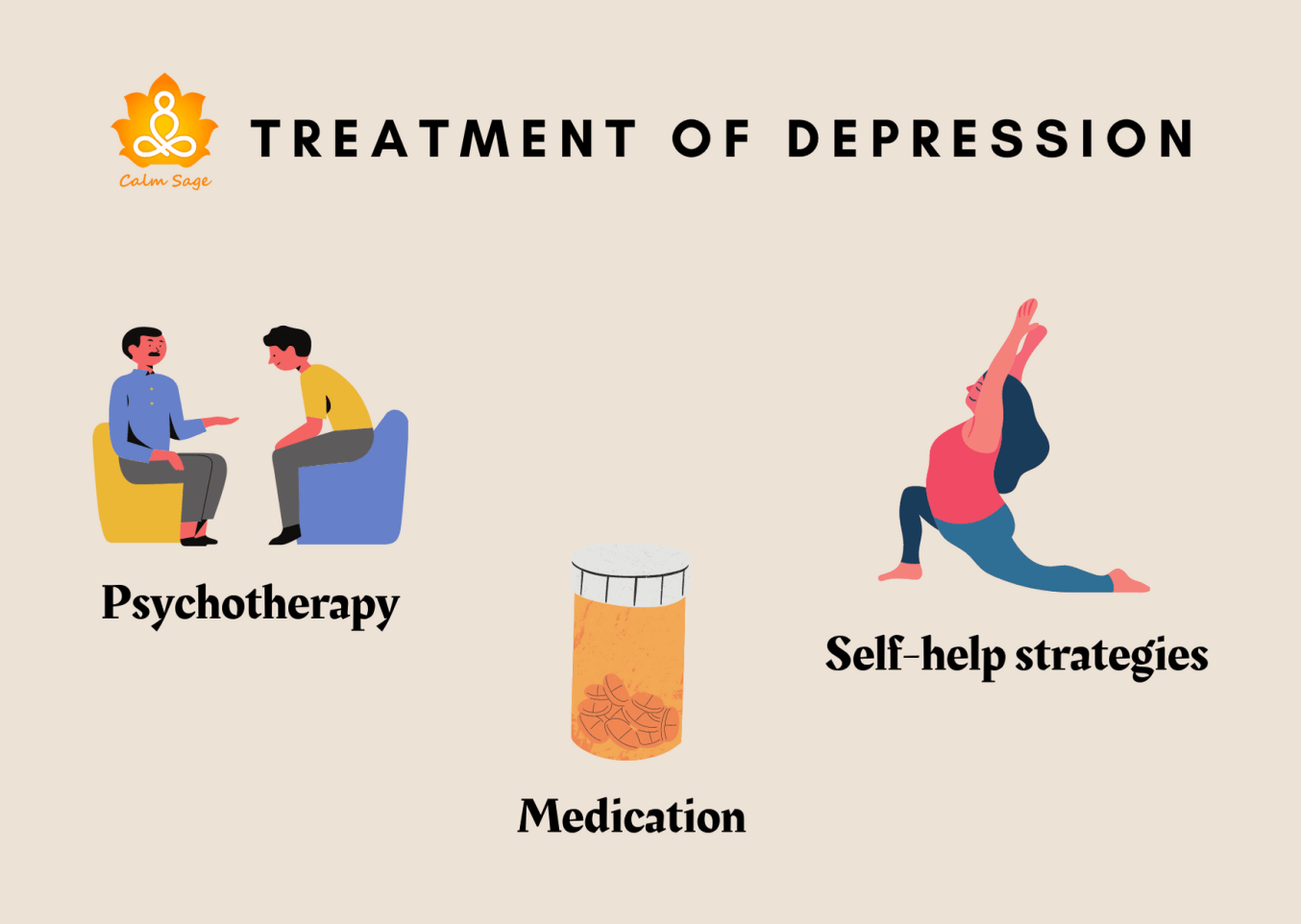
Treatment
Options
Treatment for depression varies but often includes a combination of approaches. Psychotherapy (talk therapy), medication, lifestyle changes, and alternative therapies can all be effective in managing depression. It's essential to work with a healthcare provider to determine the best treatment plan for individual needs.
1. Psychotherapy (Talk Therapy)
Cognitive-Behavioral Therapy (CBT): CBT is one of the most widely used therapies for depression. It focuses on identifying and changing negative thought patterns and behaviors that contribute to depressive symptoms. Patients learn practical skills to manage and cope with their condition.
Interpersonal
Therapy (IPT): IPT is centered around improving interpersonal relationships and
communication. It helps individuals address unresolved conflicts and social
issues that may be contributing to their depression.
Psychodynamic
Therapy: This therapy explores unconscious processes and unresolved conflicts
that may underlie depressive symptoms. It aims to increase self-awareness and
insight into one's emotions and behaviors.
Mindfulness-Based
Cognitive Therapy (MBCT): MBCT combines mindfulness techniques with cognitive
therapy. It helps individuals become more aware of their thoughts and emotions,
reducing the risk of recurrent depression.
Behavioral
Activation: This therapy focuses on increasing engagement in positive and
rewarding activities. It helps individuals counteract withdrawal and isolation,
common in depression.
2. Medication
Antidepressants: There are several classes of antidepressant medications, including selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and others. These medications work to balance neurotransmitters in the brain associated with mood regulation.
Atypical
Antidepressants: These include medications like bupropion, which work on
different neurotransmitters than SSRIs and SNRIs.
Tricyclic
Antidepressants (TCAs) and Monoamine Oxidase Inhibitors (MAOIs): These are
older classes of antidepressants used less frequently today due to potential
side effects and drug interactions. They are typically considered when other
treatments have not been effective.
3. Other
Approaches
Electroconvulsive
Therapy (ECT): ECT is a medical procedure that involves passing an electric
current through the brain to induce controlled seizures. It is considered for
severe or treatment-resistant depression when other treatments have not been
effective.
Transcranial
Magnetic Stimulation (TMS): TMS uses magnetic fields to stimulate nerve cells
in the brain. It is a non-invasive procedure and is typically used for
individuals who haven't responded well to other treatments.
Lifestyle Changes:
Lifestyle modifications, including regular exercise, a balanced diet, adequate
sleep, and stress management, can complement other treatments and improve
overall well-being.
Support Groups:
Joining a support group for depression can provide a sense of community and
understanding. Sharing experiences with others facing similar challenges can be
therapeutic.
It's important to note that the choice of treatment should be tailored to the individual's specific needs and the severity of their depression. Some individuals may benefit from a combination of therapies, while others may find relief with one approach.
Self-Help
Strategies
In addition to
professional treatment, self-help strategies can be empowering. Below are
strategies that individuals can incorporate into their daily lives to aid in
coping with depression:
1. Establish a
Routine
Create a daily
schedule that includes regular wake-up times, mealtimes, exercise, and bedtime.
Consistency can help regulate mood and provide a sense of stability.
2. Physical
Activity
Engage in regular
physical activity, even if it's light exercise like walking. Exercise releases
endorphins, which can boost mood and reduce depressive symptoms.
3. Healthy Eating
Consume a balanced
diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
Proper nutrition is essential for overall well-being.
4. Sleep Hygiene
Prioritize getting
enough quality sleep. Maintain a regular sleep schedule and create a
comfortable sleeping environment. Avoid caffeine and electronics before
bedtime.
5. Stress
Management
Practice
stress-reduction techniques such as deep breathing, meditation, mindfulness, or
yoga. These methods can help calm the mind and reduce anxiety.
6. Social
Connection
Maintain connections
with friends and loved ones. Isolation can exacerbate depression, so make an
effort to engage in social activities or reach out to a support system.
7. Limit Alcohol
and Avoid Drugs
Alcohol and
substance use can worsen depression symptoms. It's important to limit or avoid
them altogether.
8. Set Achievable
Goals
Break tasks into
smaller, manageable steps, and set realistic goals. Achieving even small
accomplishments can boost self-esteem.
9. Challenge
Negative Thoughts
Practice
recognizing and challenging negative thought patterns. Replace self-critical
thoughts with more realistic and compassionate ones.
10. Keep a Journal
Consider keeping a
journal to express thoughts and emotions. This can provide a safe outlet for
feelings and help identify patterns.
11. Engage in
Enjoyable Activities
Make time for
hobbies and activities you enjoy. Engaging in pleasurable experiences can
elevate mood and reduce symptoms of depression.
12. Seek Support
Don't hesitate to
reach out to a mental health professional, counselor, or therapist. Therapy,
whether individual or group-based, can provide effective strategies for
managing depression.
13. Educate
Yourself
Learn more about
depression through reputable sources. Understanding the condition can reduce
stigma and empower individuals to seek help.
14. Medication
Management
If prescribed
medication, adhere to the treatment plan as directed by a healthcare provider.
Medications can be an essential component of depression management.
15. Self-Compassion
Practice self-compassion
and avoid self-blame. Understand that depression is an illness and not a
personal failing.
16. Be Patient
Recovery from
depression takes time. Be patient with yourself and acknowledge progress, no
matter how small.
It's important to note that while self-help strategies can be beneficial, they are not a replacement for professional treatment when needed.
Severe or persistent depression may require the guidance of a mental health expert. Encourage individuals experiencing depression to seek help and support them in their journey toward recovery.
Conclusion
Depression is a
common and treatable condition, but it requires recognition and action. If you
or someone you know is experiencing depression, don't hesitate to seek help. In
your journey to conquer depression, remember that seeking help is a sign of
strength, not weakness. Whether through therapy, medication, or a combination
of treatments, professional support can be transformative.
Depression is a formidable foe, but you are not alone in this battle. Your mental health is worth every effort. Embrace the strategies that resonate with you, tailor them to your needs, and hold onto the belief that recovery is possible. The journey may be challenging, but it's a path toward a brighter tomorrow, where joy, fulfillment, and well-being await.
Keep moving
forward—one step at a time. You've got this.











:max_bytes(150000):strip_icc()/what-is-mild-low-grade-depression-1066956-ADD-FINAL-264dfae0d0e944a5ba7b571246947725.png)



Comments
Post a Comment