Golden Years, Gray Clouds: Understanding Depression in Older Adults
Depression is often called the "silent epidemic" among the elderly. Despite its prevalence and impact, it frequently goes unnoticed or untreated. In this blog post, we delve into the world of depression in older adults, shedding light on this critical issue, its signs, causes, and the steps we can take to address it.
The Growing
Concern: Depression Among the Elderly
Depression is a
significant mental health issue among older adults worldwide. According to the
World Health Organization (WHO), approximately 7% of the elderly population
globally experiences a depressive disorder. However, this figure is not uniform
across all regions, and it can be higher in certain populations and settings.
In Singapore, a rapidly aging population has led to an increased focus on mental health in older adults. While precise statistics can vary over time, it is estimated that around 10-15% of the elderly population in Singapore may be affected by depression or depressive symptoms. As indicated in a research paper from DukeNUS Medical School, drawing partly from a report by the Department of Statistics, Singapore, the data reveals that in 2015, 41,200 individuals aged 65 and above were residing alone in Singapore. The same source reports projections from the Singapore Ministry of Health, estimating that this number is expected to surpass double, reaching 83,000 by the year 2030.
This is a cause for concern as it not only affects the individual's quality of life but also places additional strain on healthcare systems.
Addressing the growing concern of depression among the elderly requires a multifaceted approach that includes awareness, early detection, destigmatization, and improved access to mental health care. By understanding the extent of the issue and its contributing factors, we can take steps to better support the mental well-being of older adults.
Recognizing the
Signs of Depression in Seniors
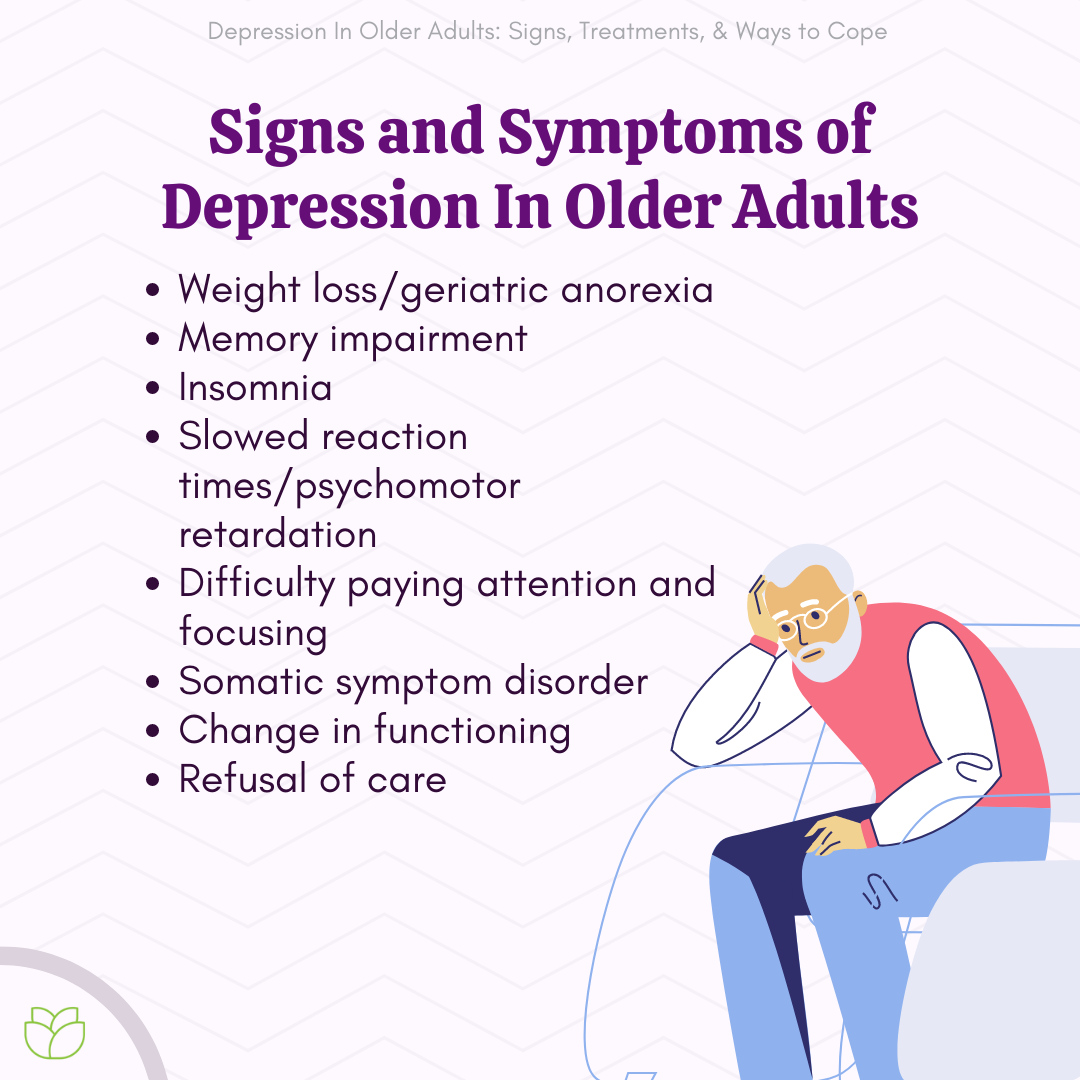
Recognizing
depression in older adults can be challenging as it often masquerades as other
conditions. Depression in older adults can often present differently from
depression in younger individuals. It's crucial to be aware of these signs and
symptoms to recognize and address depression effectively. Here are some common
signs:
Persistent Sadness:
One of the most recognizable signs is a prolonged and unexplained feeling of
sadness, emptiness, or hopelessness. It's important to note that sadness is not
the same as depression, but when it persists for an extended period, it can be
a warning sign.
Loss of Interest or
Pleasure: Older adults with depression may lose interest in activities they
once enjoyed. Hobbies, social interactions, and even family gatherings may no
longer bring joy.
Changes in Sleep
Patterns: Insomnia or oversleeping can be indicators of depression. Research
published in the Journal of the American Geriatrics Society (2014) has shown
that older adults with depressive symptoms are more likely to experience sleep
disturbances.
Appetite Changes:
Significant weight loss or gain without dietary changes or medical reasons can
be a sign. Changes in appetite can impact overall health and well-being.
Fatigue: A constant
feeling of fatigue, even after a full night's sleep, is common in seniors with
depression. It can affect their ability to perform daily tasks and maintain a
quality of life.
Physical Ailments:
Older adults with depression may frequently complain of physical symptoms like
headaches, digestive issues, or chronic pain. These can be manifestations of
their emotional distress.
Memory Problems:
Depression can contribute to cognitive difficulties, often mistakenly
attributed to dementia. Research in the journal JAMA Psychiatry (2013) suggests
that late-life depression is associated with an increased risk of dementia.
Irritability and
Restlessness: While depression is often associated with sadness, it can also
manifest as irritability, restlessness, or agitation in older adults.
Isolation: Seniors
with depression may withdraw from social activities, friends, and family,
leading to increased feelings of loneliness and isolation.
Thoughts of Death
or Suicide: It's essential to take any mention of death or suicide seriously.
Research has shown that older adults with depression are at a higher risk of
suicide attempts.
Recognizing these signs is the first step in helping seniors with depression. Since symptoms can vary among individuals, it's crucial to consider any changes in behavior, mood, or physical health. Encouraging open communication and seeking professional help when needed can significantly improve the well-being of older adults struggling with depression.
Understanding
the Causes and Risk Factors
While depression
can affect anyone, several factors make older adults more susceptible to this
condition. Understanding these causes and risk factors is crucial for effective
prevention and management.
Biological Factors: Age-related changes in the brain, such as reduced neurotransmitter production and changes in hormone levels, can contribute to depression in seniors.
Chronic Health
Conditions: Seniors often contend with chronic medical conditions like heart
disease, diabetes, or arthritis. The burden of managing these conditions can
increase the risk of depression. A study in the "Journal of the American
Geriatrics Society" (2016) underscores the link between chronic illnesses
and depression in older adults.
Medications: Some
medications commonly prescribed to seniors, including certain blood pressure
medications, can have depressive side effects.
Genetics: A family
history of depression can elevate the risk for seniors. Researchers have
identified specific genetic markers associated with late-life depression, as
reported in "Psychiatric Genetics" (2015).
Loss and Grief:
Seniors often face significant losses, such as the death of loved ones,
retirement, or declining physical health. Grief and loss can trigger or
exacerbate depression. Studies in "The American Journal of Geriatric
Psychiatry" (2017) have shown that bereavement of a loved one can result in depression.
Cognitive Decline:
Cognitive impairments, such as mild cognitive impairment (MCI) or early-stage
dementia, can coexist with depression in older adults.
Financial Stress:
Financial difficulties, especially in retirement, can lead to stress and
contribute to depression. A study in the "Journals of Gerontology: Series
B" (2017) cited the relationship between financial strain and
depressive symptoms in seniors.
Social Isolation
as a Risk Factor for Depression in Seniors
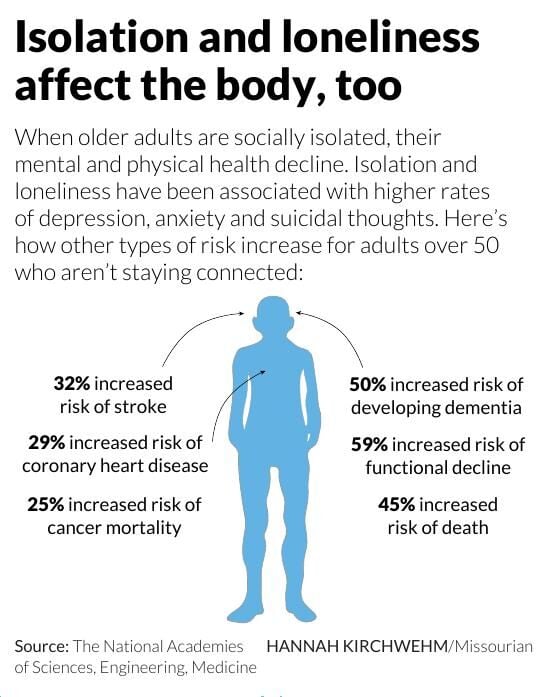
Social isolation, characterized by a lack of meaningful social interactions and connections, is a significant risk factor for depression among older adults that deserves special mention here.
Social isolation can be both an objective and subjective concept:
Objective Social
Isolation: This refers to the actual absence of social interactions, such as
limited contact with family, friends, or the community. It can be quantified by
factors like the number of social contacts, frequency of social activities, or
the size of one's social network.
Subjective Social
Isolation: Subjective social isolation relates to an individual's perception of
their social interactions. Even if an individual has social contacts, they may
still feel isolated and disconnected. Feelings of loneliness and a lack of
emotional support are common aspects of subjective social isolation.
The following
factors help explain the relationship between social isolation and depression
in seniors:
Reduced Social
Networks: As individuals age, their social networks often shrink due to factors
such as retirement, physical limitations, or the loss of friends and family
members. A study published in "Aging & Mental Health" (2018)
suggests that older adults with smaller social networks are more vulnerable to
depression.
Loneliness:
Loneliness is a subjective feeling of social isolation and disconnection. It
can lead to emotional distress and increase the risk of depression. Research in
the "Journal of Gerontology: Psychological Sciences" (2019) found that loneliness tend to occur in late-life resulting in depression.
Health
Consequences: Social isolation can have adverse effects on physical health,
including weakened immune function and higher rates of chronic illnesses. These
health issues can, in turn, contribute to depressive symptoms.
Lack of Emotional
Support: Seniors who are socially isolated may lack emotional support systems.
This absence of a trusted confidant can make it difficult for them to cope with
life's challenges, increasing their vulnerability to depression.
Cognitive Decline:
Social engagement is associated with cognitive stimulation. Research in "Aging & Mental Health (2015) reported that seniors who are
socially isolated may experience faster cognitive decline, which can lead to
depressive symptoms.
Stigmatization of
Aging: Some older adults may experience age-related stigma, which can lead to
self-isolation. Feeling devalued or excluded due to age-related stereotypes can
contribute to depressive feelings.
Barriers to Social
Participation: Physical limitations, transportation issues, or a lack of
accessible social activities can hinder seniors' ability to engage in social
interactions. These barriers can lead to increased social isolation.
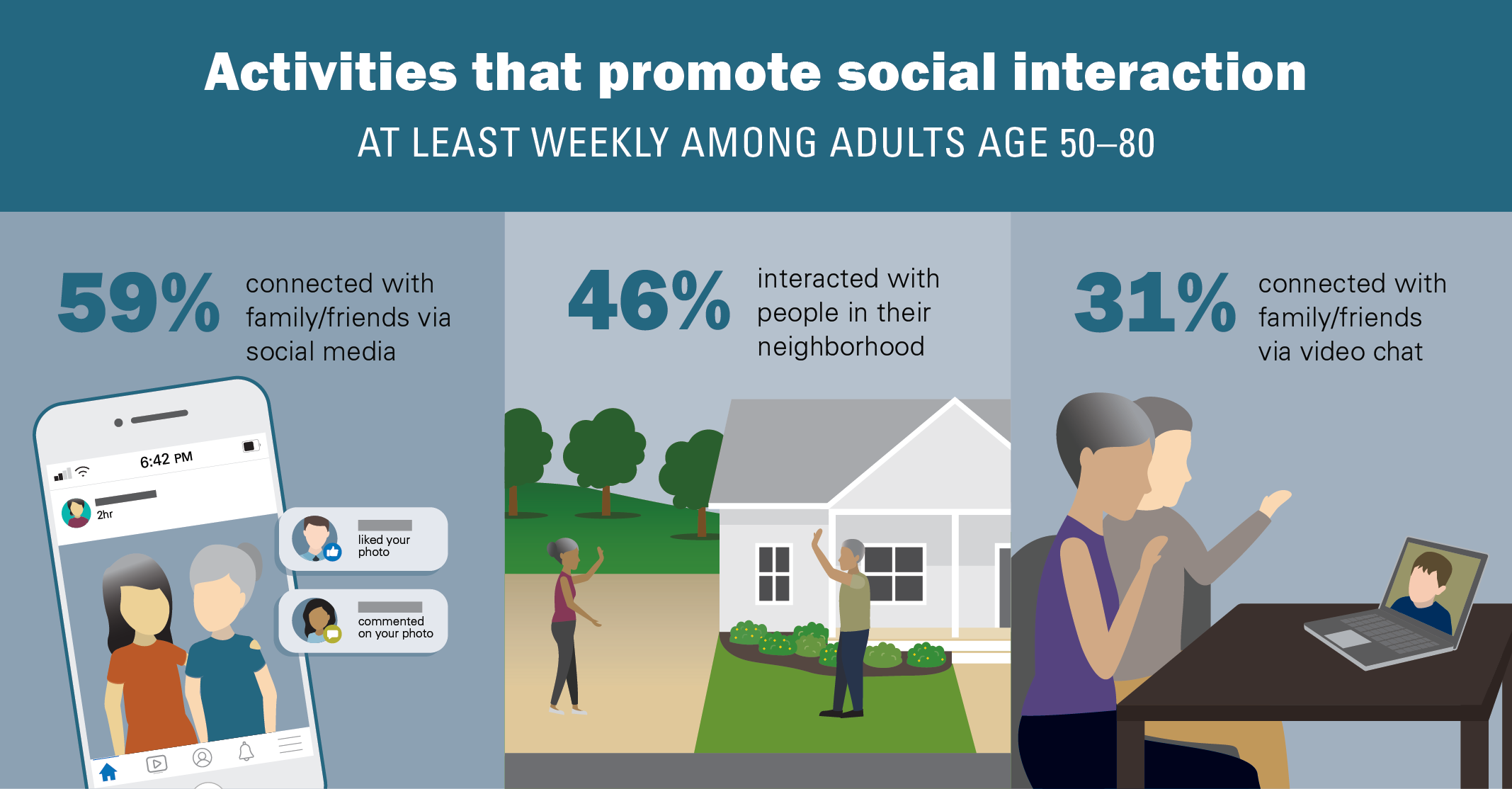
Addressing social isolation among seniors is crucial for preventing and managing depression. Interventions may include:
- Encouraging participation in community programs and activities designed for older adults.
- Promoting intergenerational connections, such as involving seniors in mentoring or volunteering with younger generations.
- Facilitating peer support groups to provide emotional connections and reduce feelings of loneliness.
- Utilizing technology for virtual social interactions, which can help bridge geographical barriers.
- Providing transportation options and support for seniors to access social events.
Treatment
Options and Strategies
Depression in seniors is a complex condition that requires careful consideration of individual needs and potential barriers to seeking help.
Here are some comprehensive treatment options and strategies:
Psychotherapy (Talk
Therapy)
Cognitive-Behavioral
Therapy (CBT): CBT is an evidence-based therapy that helps individuals identify
and challenge negative thought patterns. It's effective in treating depression
in older adults.
Interpersonal
Therapy (IPT): IPT focuses on improving relationships and social interactions,
which can be particularly beneficial for seniors dealing with isolation.
Behavioral
Activation (BA): BA helps seniors re-engage in pleasurable activities,
combatting the withdrawal and inactivity common in depression.
Medication
Management
Medication may be
prescribed when depression is severe or not responding to psychotherapy alone.
Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), are
commonly used.
Addressing concerns
about medication, such as side effects, interactions, and duration of
treatment, is crucial, as seniors may have unique medical considerations.
Collaborative Care
Collaborative care
models involve a team approach, including mental health professionals, primary
care providers, and family members. This approach can enhance engagement and
treatment outcomes.
Regular
communication between healthcare providers and seniors can help address
concerns and monitor treatment progress.
Self-Help
Strategies
Encouraging
self-help strategies can be empowering for seniors. This includes setting
achievable goals, practicing relaxation techniques, engaging in physical
activity, and maintaining a healthy diet.
Self-help
materials, such as books and online resources, can be valuable tools for
seniors to learn about their condition.
Family and Social Support
Involving family
members and close friends in the treatment process can provide essential
emotional support. It can also help ensure treatment adherence and continuity
of care.
Seniors should be
encouraged to maintain and strengthen their social connections, as increased
social engagement can be an effective strategy against depression.
Addressing
Treatment Resistance
Resistance to
treatment can be common in seniors due to factors like stigma, fear of side
effects, or reluctance to discuss their emotional struggles.
It's vital to have
open and non-judgmental conversations about these concerns. Educate seniors
about the benefits of treatment and address any misconceptions.
Telehealth and
Teletherapy
For seniors who may
have difficulty with in-person appointments, telehealth can provide access to
mental health professionals through video calls or phone consultations.
Community Resources
Encourage seniors
to explore community resources, such as senior centers, support groups, and
volunteer opportunities. These can provide social interaction and a sense of
purpose.
Regular Follow-Up
Periodic follow-up
appointments are crucial to monitor treatment progress and make adjustments as
needed. Seniors may need ongoing support to maintain their mental well-being.
Respect Autonomy
Seniors should be
active participants in their treatment decisions. Respect their autonomy and
involve them in planning their care.
Tailoring treatment
to the unique needs and preferences of seniors is essential in addressing
depression effectively. The goal is not just to alleviate symptoms but also to
improve overall well-being and quality of life. By taking a holistic and
individualized approach, seniors can receive the support they need to manage
depression and embrace a healthier, more fulfilling life.
Conclusion: Aging Gracefully and Mentally Healthy
In conclusion,
depression is a prevalent and often undetected issue among the elderly.
Recognizing the signs, understanding the causes, and seeking help are essential
steps in addressing this challenge. By fostering a supportive environment and
promoting mental wellness, we can help our elderly loved ones age gracefully
and maintain their mental health.







Comments
Post a Comment