Understanding Stroke: A Silent Predator in Our Midst
Imagine a morning like any other. The sun is casting its gentle glow through the curtains, and you're preparing for the day ahead. But in an instant, the world as you know it can change, and the life you've built can be shattered. That's the power of a stroke, a silent predator lurking in the shadows, ready to strike without warning.
For many, the word
"stroke" remains distant, something that happens to others, until
that fateful moment when it becomes deeply personal. A stroke is not just a
medical term; it's a life-altering event. It doesn't discriminate based on age,
gender, or background. It takes lives, shatters dreams, and leaves families in
agony.
In the blink of an
eye, the ability to speak, to move, to live independently can be snatched away.
It leaves survivors with scars that run deeper than what meets the eye. It can
leave us grieving for the life we once had.
But it doesn't have
to be this way. We have the power to change the course of this devastating
disease, to protect our loved ones, and to safeguard our own well-being. We can
become vigilant in the face of this silent terror, arming ourselves with
knowledge and resilience. By understanding the risks and embracing preventive
measures, we can face the future with courage and ensure that stroke remains a
word on a page, not a nightmare in our lives.
Join us in this journey to understand stroke, its causes, symptoms, and most importantly, how we can prevent it from ever knocking on our doors.
What Is a
Stroke?
A stroke is a
sudden disruption of blood flow to the brain. There are three main types of
stroke:
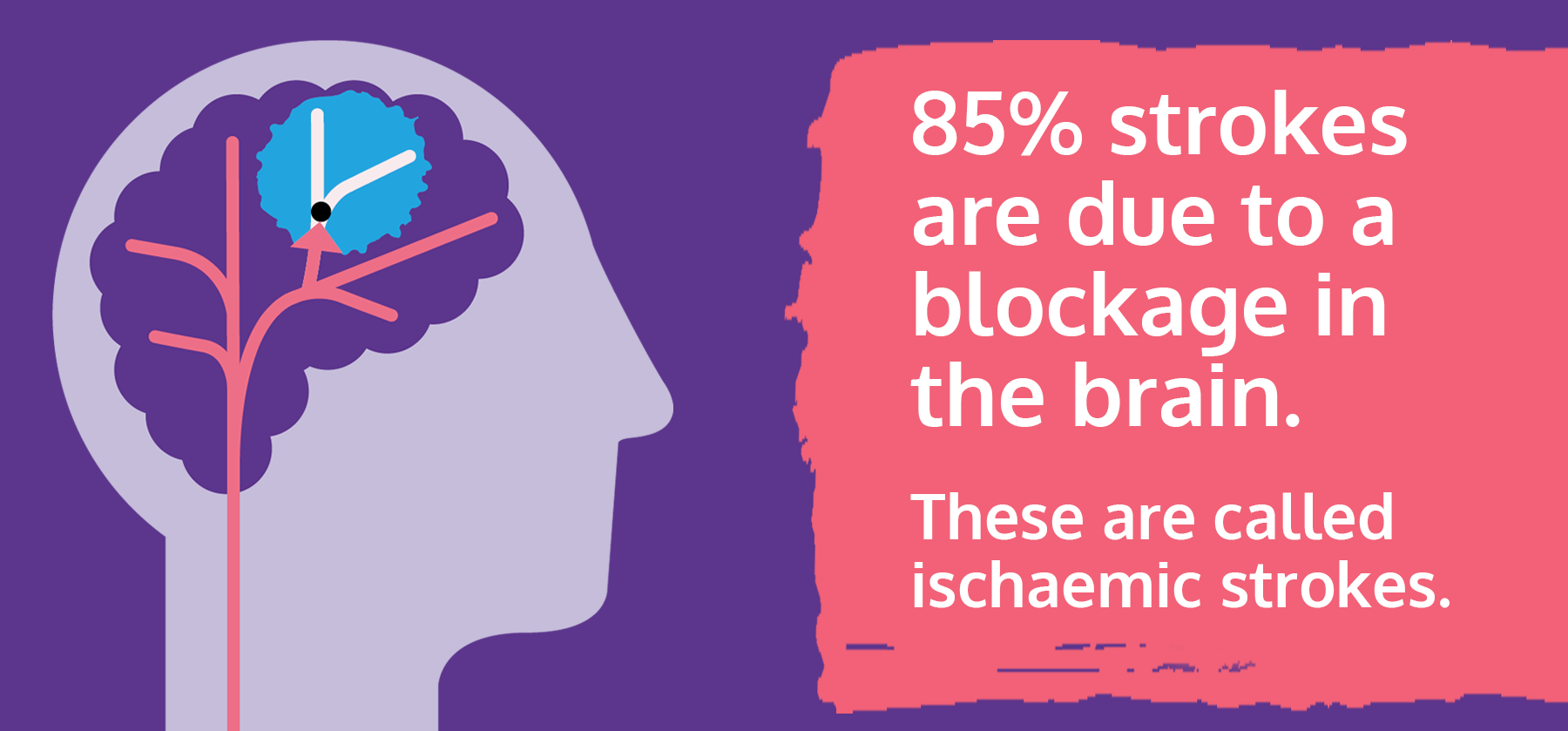
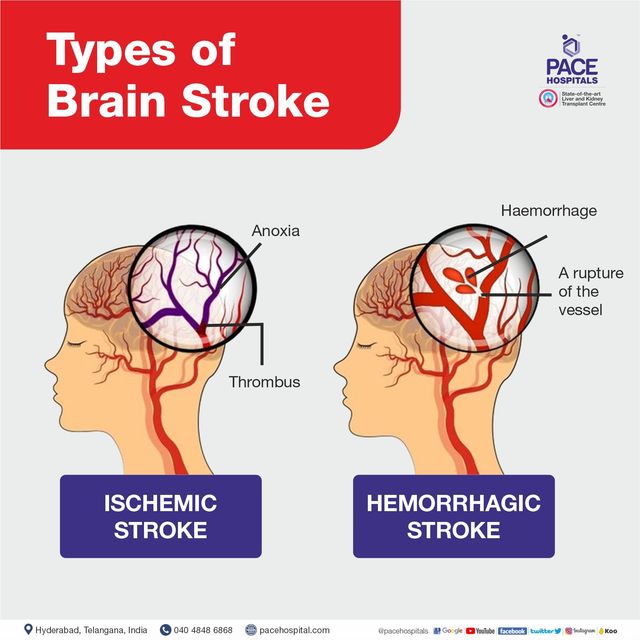
Ischemic Stroke: Ischemic
strokes are the most common type, accounting for approximately 87% of all
strokes. They occur when a blood clot or plaque blocks a blood vessel in the
brain, cutting off the blood supply to a specific area. Without an adequate
blood supply, brain cells begin to die, leading to neurological deficits.
Hemorrhagic Stroke: Hemorrhagic strokes result from the rupture of a blood vessel in the brain. This leads to bleeding within the brain tissue or into the surrounding spaces. Hemorrhagic strokes can be further categorized into intracerebral hemorrhages (bleeding within the brain) and subarachnoid hemorrhages (bleeding into the space surrounding the brain).
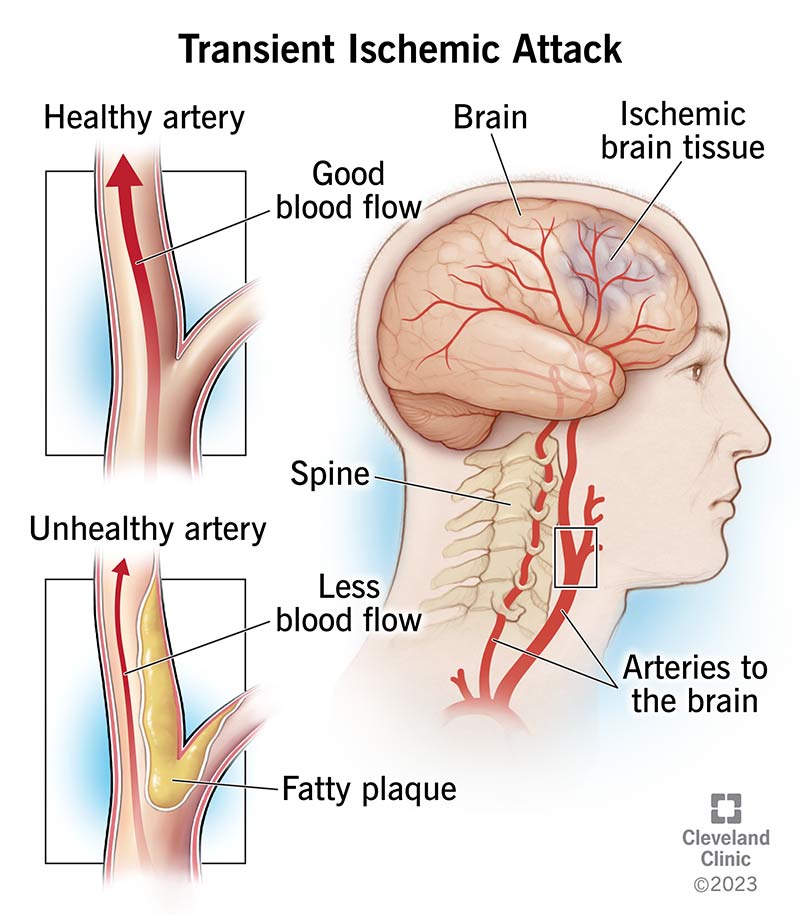
Transient Ischemic Attack (TIA): Often called a "mini-stroke," a TIA is caused by a temporary blockage. It produces stroke-like symptoms that resolve within 24 hours, typically lasting only a few minutes.
TIAs are warning signs of a potential full-blown stroke and should be taken seriously. Although it doesn't cause permanent damage, it serves as a warning sign of a potential major stroke.
Prevalence of
Stroke
Globally, strokes
are alarmingly common. According to the World Health Organization (WHO), stroke
is the second leading cause of death and the third leading cause of disability
worldwide. It's a sobering statistic that should make us pause and pay
attention.
According to the
Ministry of Health, stroke in Singapore is the fourth leading cause of death,
with a prevalence of 4% among adults aged 50 years and above. The number of
people having stroke is on the rise in Singapore, especially among adults aged
40 to 59 years. Stroke strikes about 8,300 people here every year – around 1 in
4 are under 60 years old, when they are reaching the peak of their careers and
busy caring for family members.
Causes and Risk Factors
Several well-documented risk factors contribute to the development of stroke. Understanding these risk factors is essential for stroke prevention and management.
Here are some of the most common risk factors:
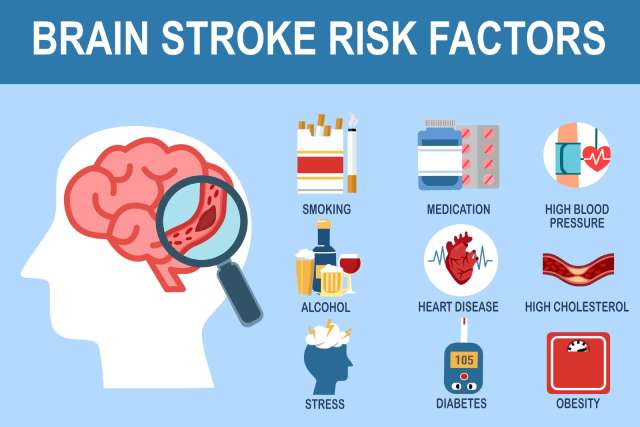
Hypertension (High
Blood Pressure): Hypertension is a major risk factor for both ischemic and
hemorrhagic strokes. It damages blood vessels and increases the likelihood of
blood clots and vessel ruptures. A study published in The Lancet Neurology
(O'Donnell et al., 2010) found that reducing blood pressure significantly
lowers the risk of stroke.
Diabetes:
Individuals with diabetes are at an increased risk of stroke. High blood sugar
levels can damage blood vessels over time. A study in Diabetologia (Sarwar et
al., 2010) reported the strong association between diabetes and stroke risk.
High Cholesterol:
Elevated levels of low-density lipoprotein (LDL) cholesterol can lead to
atherosclerosis, a condition where fatty deposits accumulate in arteries. A
meta-analysis in the American Heart Journal (Oei et al., 2006) established the
link between high cholesterol and ischemic stroke.
Smoking: Smoking is
a well-established risk factor for stroke. The toxins in tobacco smoke can
damage blood vessels and increase the risk of blood clots. Research published
in Stroke (Hassan et al., 2018) highlights the harmful effects of smoking on stroke
risk.
Atrial
Fibrillation: Atrial fibrillation, an irregular heart rhythm, can lead to blood
clots that may cause strokes. Studies like the one in The New England Journal
of Medicine (Wolf et al., 1991) emphasize the association between atrial fibrillation
and stroke risk.
Sedentary
Lifestyle: Lack of physical activity and a sedentary lifestyle can contribute
to several risk factors for stroke, including obesity, hypertension, and
diabetes. A study in Stroke (Lackland et al., 2014) underscores the importance
of physical activity in stroke prevention.
Excessive Alcohol
Consumption: Heavy alcohol consumption can raise blood pressure and increase
the risk of hemorrhagic strokes.
Obesity: Obesity is
linked to various risk factors, such as hypertension, diabetes, and high
cholesterol, which collectively increase the likelihood of stroke.
It's important to
note that addressing these risk factors through lifestyle modifications and
medical management can significantly reduce the risk of stroke.
Recognizing the
symptoms of a stroke is crucial because early intervention can make a
significant difference in the outcome. Strokes can manifest suddenly, and they
often have distinct signs, which can be remembered using the acronym
"FAST": Face, Arms, Speech, and Time.
Face Drooping: One
of the most common signs of a stroke is the sudden drooping of one side of the
face. When a person tries to smile, their smile may appear uneven, or one side
of the mouth may sag.
Arm Weakness: Another key symptom is sudden weakness or numbness in one or both arms. A person may have difficulty raising both arms, and one arm may drift downward when they try to raise them.
Speech Difficulty:
Speech problems are often seen in stroke patients. They may have trouble
speaking, and their speech may become slurred. They may also struggle to
understand simple sentences or find the right words.
Time to Call for
Help: The "T" in FAST stands for "Time." If you observe any
of these signs, it's crucial to act quickly. Time is of the essence in stroke
cases, as certain treatments must be administered within a specific time frame
to be effective.
Sudden severe
headache: This is more common in hemorrhagic strokes.
Trouble seeing in
one or both eyes: Vision may become blurred or blackened.
Dizziness, loss of
balance, or difficulty walking: This may result from damage to the brain's
coordination centers.
Confusion or
changes in mental status: Some stroke victims may become disoriented or have
difficulty understanding information.
It's important to
note that not all these symptoms may be present, and they can vary in severity.
If you or someone you are with experiences any of these symptoms, even if they
seem to improve, it's crucial to call emergency services immediately. Early
medical intervention can help minimize the damage caused by a stroke.
Remember,
"FAST" is a quick and simple way to recognize stroke symptoms, but
don't hesitate to call for help if you notice any of the signs mentioned, even
if they don't fit the "FAST" acronym.
Understanding these
symptoms and acting swiftly can make a significant difference in the treatment
and recovery of a stroke.
Prevention
Blood Pressure
Management: High blood pressure (hypertension) is one of the most significant
risk factors for stroke. Regularly monitor your blood pressure, and if it's
high, work with your healthcare provider to keep it within a healthy range.
Lifestyle changes like a balanced diet, regular exercise, and reducing salt
intake can help manage blood pressure.
Healthy Eating: A
diet rich in fruits, vegetables, whole grains, and lean proteins can contribute
to better heart health and reduce stroke risk. Avoid excessive saturated fats,
trans fats, and cholesterol. Maintain a healthy weight, and watch your calorie
intake.
Regular Exercise: Physical activity is essential for maintaining cardiovascular health. Aim for at least 150 minutes of moderate-intensity exercise per week, such as brisk walking or swimming. Physical activity can help control weight, lower blood pressure, and improve overall fitness.
Smoking Cessation:
Smoking significantly increases the risk of stroke. If you smoke, quitting is
one of the most effective ways to reduce your risk. Seek support from smoking
cessation programs and healthcare professionals.
Moderate Alcohol
Consumption: Excessive alcohol consumption can raise blood pressure and
contribute to stroke risk. If you choose to drink, do so in moderation, which
generally means up to one drink per day for women and up to two drinks per day
for men.
Manage Diabetes: If
you have diabetes, maintaining good control over your blood sugar levels is
essential. Regular monitoring, a healthy diet, and medication as prescribed by
your healthcare provider can help manage diabetes and reduce stroke risk.
Cholesterol
Control: High levels of LDL cholesterol (the "bad" cholesterol) can
contribute to arterial plaque buildup, increasing the risk of stroke. Work with
your healthcare provider to manage your cholesterol levels through diet,
exercise, and, if necessary, medication.
Regular Health
Checkups: Regular checkups with your healthcare provider can help identify and
manage risk factors early. These visits provide an opportunity to assess and
discuss your overall health, including blood pressure, cholesterol, and other
stroke risk factors.
Atrial Fibrillation
Management: Atrial fibrillation, an irregular heartbeat, can increase stroke
risk. If you have this condition, work closely with your healthcare provider to
manage it and reduce the risk of blood clots that could lead to a stroke.
Antiplatelet
Medications: Some individuals with specific risk factors may benefit from
medications that help prevent blood clots. Your healthcare provider will
determine if these medications are appropriate for you.
Lifestyle
Modification: Lifestyle changes, such as stress management and getting adequate
sleep, can also contribute to stroke prevention. Chronic stress and lack of
sleep can negatively affect cardiovascular health.
By incorporating these strategies into your daily life, you can significantly reduce your risk of stroke. Remember, stroke prevention is a lifelong commitment to maintaining a healthy lifestyle and managing medical conditions effectively. If you have specific concerns or risk factors, consult your healthcare provider for personalized guidance on stroke prevention.
Diagnosis
Physical
Examination: When a person arrives at the hospital with suspected stroke,
healthcare providers conduct a physical examination to assess the person's
symptoms, vital signs, and neurological functions. They will also obtain a
medical history to identify risk factors.
Imaging Tests: Imaging plays a crucial role in diagnosing the type of stroke and its location. The primary imaging tests used include:
The primary imaging
tests used include:
CT (Computed
Tomography) Scan: A CT scan can quickly identify whether a stroke is ischemic
or hemorrhagic, helping determine the appropriate treatment.
MRI (Magnetic
Resonance Imaging): An MRI provides detailed images of the brain, helping to
evaluate the extent of damage and identify smaller or earlier strokes.
CT Angiography and
MR Angiography: These tests can help identify blocked or narrowed blood vessels
in the brain.
Blood Tests: Blood tests can reveal important information about the person's overall health and may help identify underlying conditions that increase the risk of stroke.
Electrocardiogram
(ECG or EKG): An ECG records the heart's electrical activity and can identify
irregular heart rhythms, such as atrial fibrillation, which is a significant
risk factor for stroke.
Cerebral
Angiography: In some cases, a cerebral angiography may be performed to get
detailed images of blood vessels in the brain.
Treatment
Ischemic Stroke:
Ischemic strokes, which result from a blocked artery, are often treated with
the following approaches:
- Clot-Busting Medications (Thrombolytics): Tissue plasminogen activator (tPA) is an example of a clot-busting medication that can be administered intravenously to dissolve the clot and restore blood flow.
- Endovascular Procedures: These procedures involve threading a catheter through blood vessels to the site of the clot, where a device can be used to physically remove or break up the clot.
- Antiplatelet and Anticoagulant Medications: These medications may be prescribed to prevent further clot formation and manage underlying conditions, such as atrial fibrillation.
Hemorrhagic Stroke:
Hemorrhagic strokes are treated differently, focusing on controlling bleeding
and reducing pressure on the brain:
- Surgery: Depending on the source of bleeding, surgery may be necessary to repair an aneurysm or remove a blood clot.
- Medication Management: Medications to control blood pressure, reduce swelling, and prevent seizures are commonly used in hemorrhagic stroke treatment.
Rehabilitation:
After the initial treatment, stroke survivors often require extensive
rehabilitation to regain lost functions and improve their quality of life.
Rehabilitation may include physical therapy, occupational therapy, speech
therapy, and psychological support.
Secondary
Prevention: Stroke survivors are often prescribed medications to manage risk
factors, such as antihypertensives, statins, and anticoagulants. Lifestyle
modifications, including dietary changes and regular exercise, are also crucial
for preventing recurrent strokes.
Supportive Care: Stroke care may include various supportive measures, such as speech therapy, counseling, and support for activities of daily living.
Long-Term
Management: Managing the underlying causes of stroke, such as hypertension or
diabetes, is an essential part of long-term care.
It's crucial for
individuals experiencing stroke symptoms to seek immediate medical attention,
as the effectiveness of treatment depends on early intervention. Rapid and
appropriate treatment can improve the chances of recovery and minimize
long-term disability. Stroke care is often provided by a multidisciplinary team
of healthcare professionals, including neurologists, neurosurgeons, and
rehabilitation specialists, working together to create a comprehensive
treatment plan.
Recovery Process
Recovery after a
stroke can be challenging, and it often involves physical, speech, and
occupational therapy. However, the extent of recovery varies among individuals.
Up to a third of stroke patients
recover fully, a third recover partially, and a third do not recover at all.
About 10% to 20% may not survive the early period after the stroke. Recovery
takes time. Most recovery occurs in the first 3 to 6 months, but it may
continue slowly for many years.
There is a 5% to 15% chance a year of the stroke recurring. To reduce the chance of another stroke, all medications should be taken regularly and smoking must be stopped.
The long-term
impact of a stroke can be profound, affecting every aspect of an individual's
life. Physical, emotional, and cognitive changes are common after a stroke.
Conclusion
A stroke is a
life-altering event that affects millions of people worldwide. Its devastating
impact reminds us of the fragility of life. But, with awareness, lifestyle
changes, and timely medical interventions, we can reduce the risk and
consequences of stroke. This article has sought to shed light on this silent
predator, equipping you with the knowledge to take control of your health and
prevent stroke from becoming a tragic chapter in your life.

:max_bytes(150000):strip_icc()/senior-man-patient-sleeping-with-her-wife-sitting-onside-in-hospital-670911949-5944612e3df78c537b1c86ea.jpg)








:max_bytes(150000):strip_icc()/coping-with-stroke-4158490_final-1b78f0205e004bb3877e20610da2b03c.jpg)

Comments
Post a Comment