Understanding Alzheimer's Disease: Causes, Symptoms, and Care
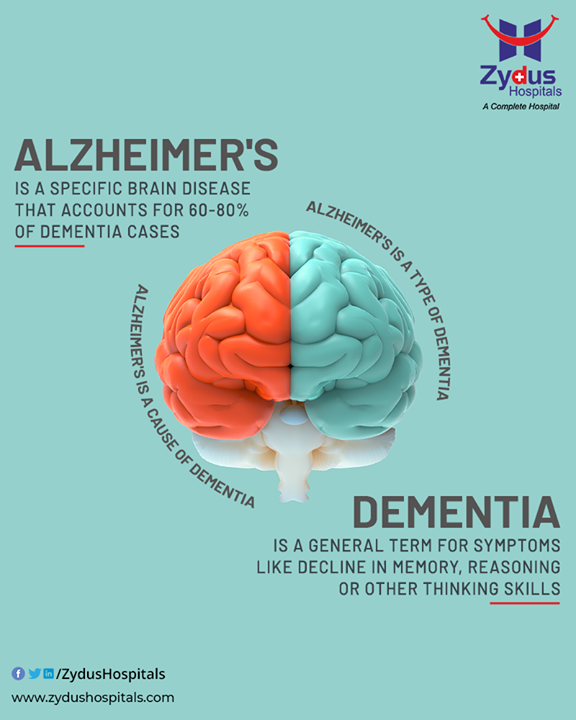
Alzheimer's disease is a topic that affects millions of individuals and their families worldwide. This neurodegenerative condition is the most common cause of dementia, and understanding its causes, symptoms, and care strategies is essential for both those directly affected and their caregivers. In this blog post, we will delve into the intricacies of Alzheimer's disease, shedding light on its fundamental aspects.
Definition and Basics
Alzheimer's disease
is a progressive brain disorder that impacts memory, thinking, and behavior. It
slowly erodes cognitive function, making everyday tasks challenging for those
affected. It is a type of neurodegenerative diseases and is
characterized by the abnormal accumulation of protein deposits in the brain,
leading to the death of nerve cells and the gradual deterioration of cognitive
function. While it typically occurs in older adults, it's important to note
that it's not a normal part of aging.
Alzheimer's disease
is a global health concern with a staggering prevalence. According to the World
Alzheimer Report 2021, an estimated 55 million people worldwide are living with
dementia, and Alzheimer's disease accounts for the majority of dementia cases.
To put this into perspective, someone in the world develops dementia every
three seconds.
In the United
States alone, Alzheimer's disease affects over 6 million individuals, making it
the sixth leading cause of death. It's important to note that Alzheimer's
disease is not limited to older adults, although advancing age is the most
significant risk factor. Early-onset Alzheimer's can manifest in individuals as
young as their 30s and 40s, although it is relatively rare.
The impact of Alzheimer's disease extends beyond the individual diagnosed. It places an immense emotional, physical, and financial burden on families and caregivers. The demands of caregiving, coupled with the progressive nature of the disease, can result in significant stress and burnout for those providing care.
Understanding the
prevalence and impact of Alzheimer's disease underscores the urgency of research,
early detection, and effective care strategies. As the global population ages,
the number of individuals living with Alzheimer's is expected to rise
significantly, making it an issue of increasing importance for healthcare
systems and society as a whole.
Causes and Risk
Factors
The exact cause of
Alzheimer's disease remains elusive, but both genetic and environmental factors
are believed to play a role. Age is the most significant risk factor, with the
risk doubling every five years after the age of 65. Family history and certain
lifestyle choices, such as smoking and a sedentary lifestyle, also increase the
risk.
Researchers
continue to explore these factors to gain a deeper understanding of the
disease. Here are some key aspects to consider:
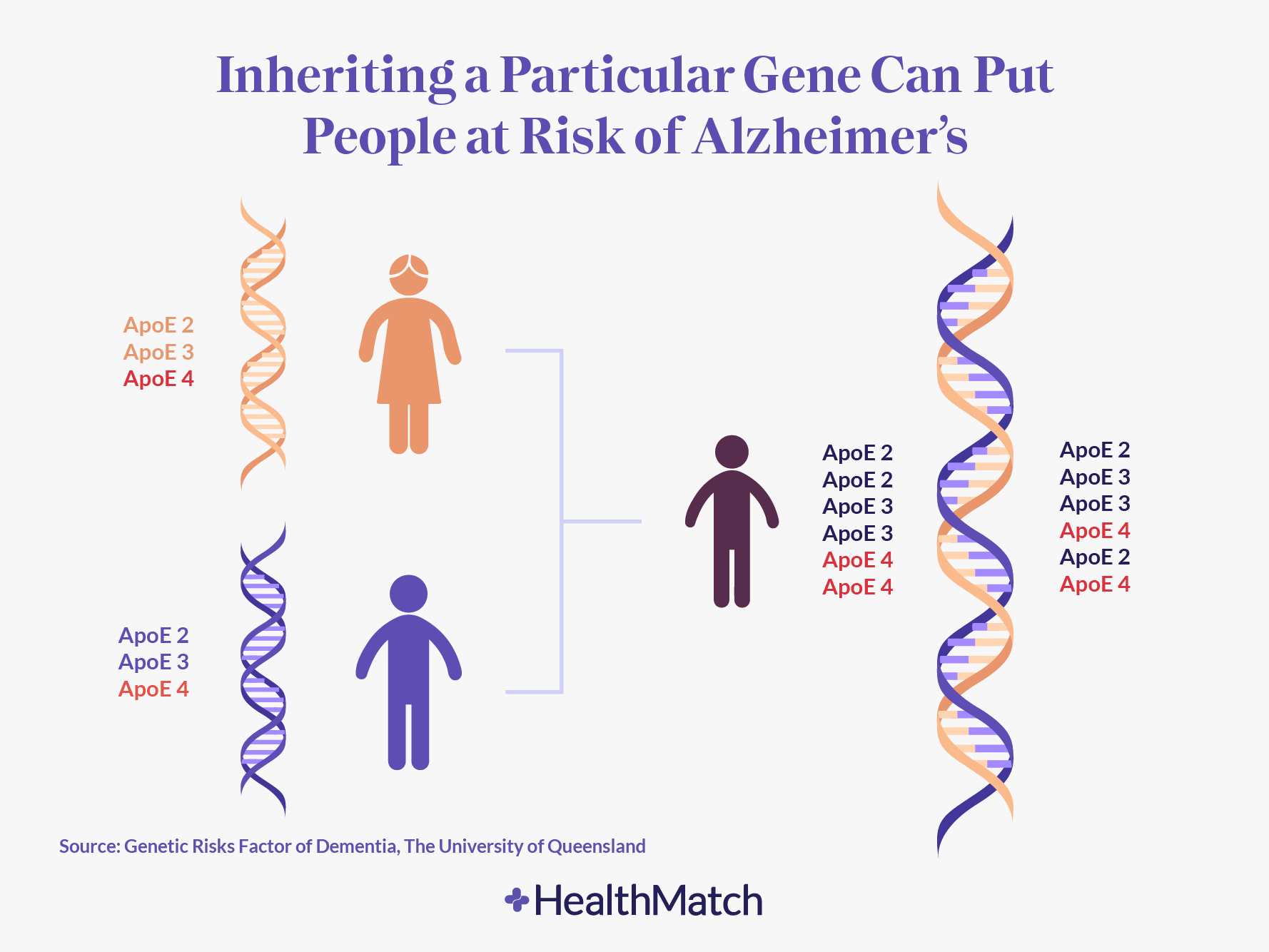
1. Genetic Factors
APOE Gene: One of
the most well-established genetic risk factors is the apolipoprotein E (APOE)
gene. According to researchers, there are three common variants of this gene:
APOE ε2, APOE ε3, and APOE ε4. APOE ε4 is associated with an increased risk of
Alzheimer's disease. Individuals who inherit one copy of APOE ε4 have a higher
risk, while those with two copies face an even greater risk (Corder at al,
1993). However, it's important to note that having APOE ε4 does not guarantee
that an individual will develop Alzheimer's.
Other Genetic Factors: Beyond APOE, researchers (Rogaeva et al, 1995) have identified several other genes associated with Alzheimer's disease. These include presenilin 1 (PSEN1), presenilin 2 (PSEN2), and amyloid precursor protein (APP) mutations. These rare genetic mutations lead to early-onset Alzheimer's disease, typically occurring before the age of 65.
2. Age
Advancing Age: Age
is the most significant non-modifiable risk factor for Alzheimer's disease. The
risk of developing Alzheimer's increases as individuals get older. While the
disease can affect people in their 30s or 40s (early-onset Alzheimer's), the vast
majority of cases occur in individuals over the age of 65 (Brookmeyer et al.,
2011)
3. Lifestyle
Factors
Cardiovascular Health: Emerging research suggests a strong link between cardiovascular health and Alzheimer's disease. Conditions such as hypertension, diabetes, obesity, and high cholesterol may increase the risk (Livingston et al, 2017).
Diet and Exercise: A growing body of evidence suggests that a heart-healthy diet (e.g., the Mediterranean diet) and regular physical activity may help reduce the risk of Alzheimer's disease (Scarmeas et al, 2009).
Education and Cognitive Engagement: Higher levels of education and lifelong cognitive engagement have been associated with a reduced risk of Alzheimer's disease (Valenzuela & Sachdev, 2006).
Head Trauma: There
is evidence that severe head trauma, especially when accompanied by loss of
consciousness, may be a risk factor for Alzheimer's disease (Fleminger et al
2003).
It's important to note that while these risk factors are associated with a higher likelihood of developing Alzheimer's disease, they do not guarantee its onset. Additionally, research is ongoing to better understand the interplay between genetics, lifestyle, and environmental factors in Alzheimer's disease development.
Stages of Alzheimer's
Disease
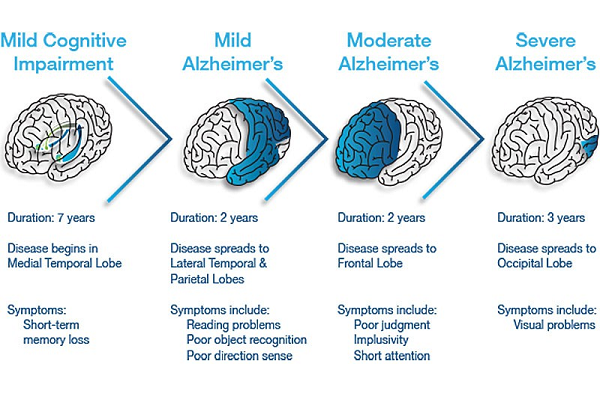
Alzheimer's disease
typically progresses through distinct stages, each characterized by specific
cognitive and functional changes. It's important to note that not all
individuals will experience these stages in the same way or at the same rate.
The stages are often described as follows:
1. Preclinical
Alzheimer's Disease
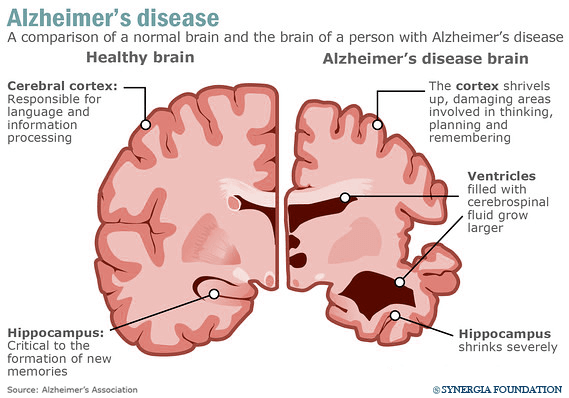
This
stage occurs before noticeable symptoms appear. In preclinical Alzheimer's,
biological changes such as the accumulation of amyloid plaques and tau tangles
in the brain may be underway, but cognitive function remains intact.
2. Mild Cognitive
Impairment (MCI) Due to Alzheimer's Disease
In
this stage, individuals may experience mild cognitive changes that are
noticeable to themselves and close family members, but these changes do not
significantly interfere with daily life.
3. Mild Alzheimer's
Disease
Mild
Alzheimer's is characterized by more pronounced cognitive deficits, including
memory problems, difficulty with language, and challenges with problem-solving.
Individuals may also experience mood swings and personality changes.
4. Moderate
Alzheimer's Disease
The
moderate stage is marked by significant cognitive decline. Individuals may have
difficulty recognizing loved ones, experience disorientation, and require
assistance with daily activities.
5. Severe
Alzheimer's Disease
In the
severe stage, individuals are profoundly cognitively impaired. They may lose
the ability to communicate, become bedridden, and require round-the-clock care.
Recognizing the
Symptoms
Recognizing
Alzheimer's disease in its early stages can be challenging as symptoms are
often subtle. These may include memory lapses, difficulty completing familiar
tasks, and confusion about time or place. One of the most common early signs of
Alzheimer's is memory loss that disrupts daily life. Individuals may forget
recently learned information, important dates, or appointments (McKhann et al,
2011).
Difficulty
Completing Familiar Tasks: People with Alzheimer's may have trouble completing
tasks they've done their whole lives, such as cooking a meal or managing
finances (Albert et al, 2011). This can lead to frustration and confusion.
Confusion About Time or Place: Individuals may become disoriented and lose track of dates, seasons, or their current location (Dubois et al, 2007).
Challenges with Problem-Solving: Alzheimer's can impair an individual's ability to develop and follow a plan. They may struggle with tasks like following a recipe or keeping track of bills (Albert et al, 2011).
Difficulty Finding
Words: Language problems can arise, making it challenging for individuals to
join or follow conversations (Dubois et al, 2014). They may struggle to find
the right word or repeat themselves.
Progression of Symptoms
As Alzheimer's
disease advances, symptoms intensify. Individuals may experience mood swings,
agitation, and a decline in their ability to communicate effectively.
Behavioral and psychological symptoms can pose significant challenges for both
the affected individual and their caregivers.
Mood and
Personality Changes: As Alzheimer's advances, mood swings and personality
changes can occur. Individuals may become anxious, agitated, or withdrawn (Robert
et al, 2006).
Loss of Initiative:
Apathy and a decreased interest in initiating activities are common in later
stages of Alzheimer's (Robert et al, 2006). Individuals may require prompting
to engage in daily routines.
Wandering and
Getting Lost: Individuals with Alzheimer's may wander and become disoriented,
potentially putting themselves in unsafe situations (Algase et al 2008).
Trouble with Visual
Perception: Perceptual difficulties can lead to problems with reading, judging
distances, and identifying colors and contrast (Algase et al 2008).
Sleep Disturbances: Alzheimer's often disrupts sleep patterns, leading to frequent nighttime awakenings and daytime drowsiness (McCurry et al, 1999).
These symptoms highlight the progressive and multifaceted nature of Alzheimer's disease. It's important to remember that Alzheimer's affects each individual differently, and the rate at which symptoms progress can vary. Early recognition and diagnosis are crucial to providing appropriate care and support to individuals and their families. Additionally, ongoing research continues to shed light on the complexities of Alzheimer's symptoms and management strategies.
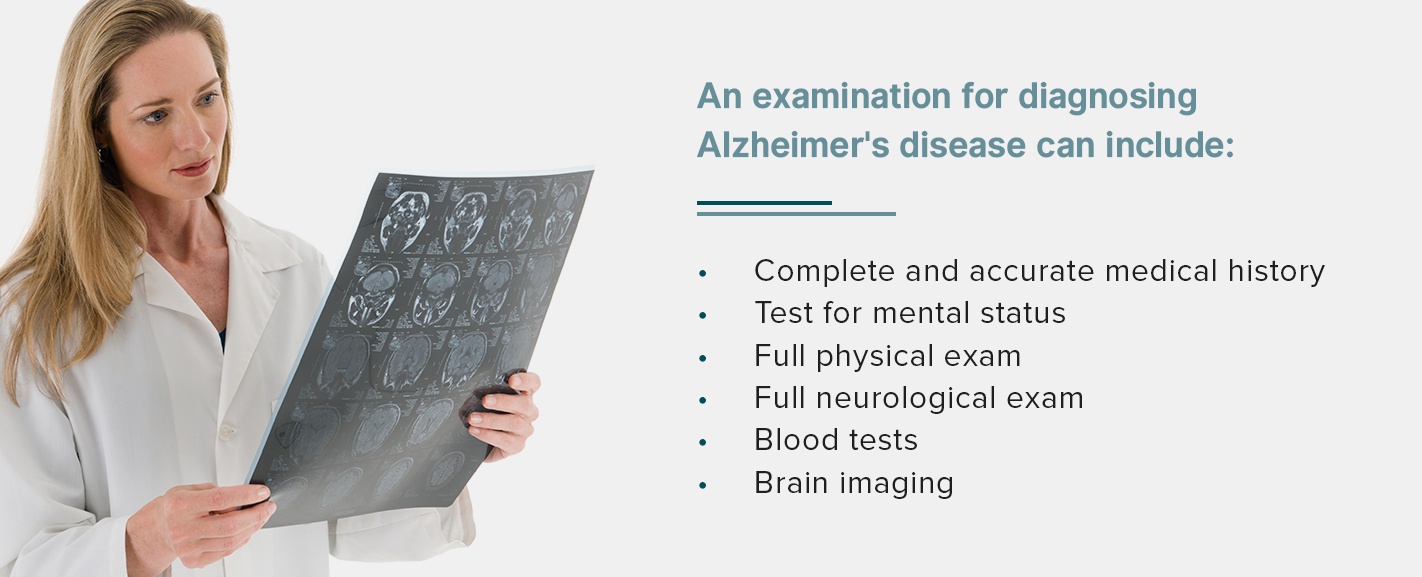
Diagnosis and
Medical Evaluation
Diagnosing
Alzheimer's disease involves a thorough medical evaluation, including physical
and neurological exams, cognitive assessments, and medical history reviews.
Brain imaging and laboratory tests may also be performed.
Clinical
Assessment: The diagnostic journey often begins with a thorough clinical
assessment by a healthcare provider. This assessment includes a detailed
medical history, cognitive tests, and discussions with the individual and their
family regarding symptoms and changes in daily functioning.
Neuropsychological
Testing: Neuropsychological tests are specialized assessments that evaluate cognitive
function in detail. They examine memory, attention, language, and
problem-solving abilities. Common neuropsychological tests include the
Mini-Mental State Examination (MMSE) and the Montreal Cognitive Assessment
(MoCA).
Brain Imaging: Brain imaging techniques are crucial for diagnosis. Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans can reveal structural changes in the brain. Positron Emission Tomography (PET) scans and Single Photon Emission Computed Tomography (SPECT) scans can detect abnormal protein deposits, like amyloid plaques and tau tangles, associated with Alzheimer's.
Cerebrospinal Fluid
Analysis: In some cases, a lumbar puncture (spinal tap) may be performed to
analyze cerebrospinal fluid. This can help detect biomarkers associated with
Alzheimer's, such as elevated levels of tau and decreased levels of amyloid
beta.
Early diagnosis offers several advantages. It allows for better access to available treatments and interventions that can help manage symptoms and maintain quality of life. Additionally, it empowers individuals and their families to plan for the future.
Better Treatment Options: Early diagnosis provides individuals and their families with more treatment options. While there is no cure for Alzheimer's, medications like cholinesterase inhibitors (e.g., donepezil) and memantine can help manage symptoms and slow cognitive decline when started early.
Planning and
Support: An early diagnosis allows individuals and families to plan for the
future, make informed decisions about care, and access available support
services, such as caregiver resources and community programs.
Participation in
Research: Early diagnosis can open doors to participation in clinical trials
and research studies, contributing to our understanding of Alzheimer's and
potential treatment advancements.
It's important to
emphasize that diagnosing Alzheimer's disease is a complex and comprehensive
process that requires the expertise of healthcare professionals. Early
recognition and intervention can significantly impact an individual's quality
of life and their ability to plan for the future. Researchers continue to
refine diagnostic methods and develop new tools to aid in the early detection
of Alzheimer's disease.
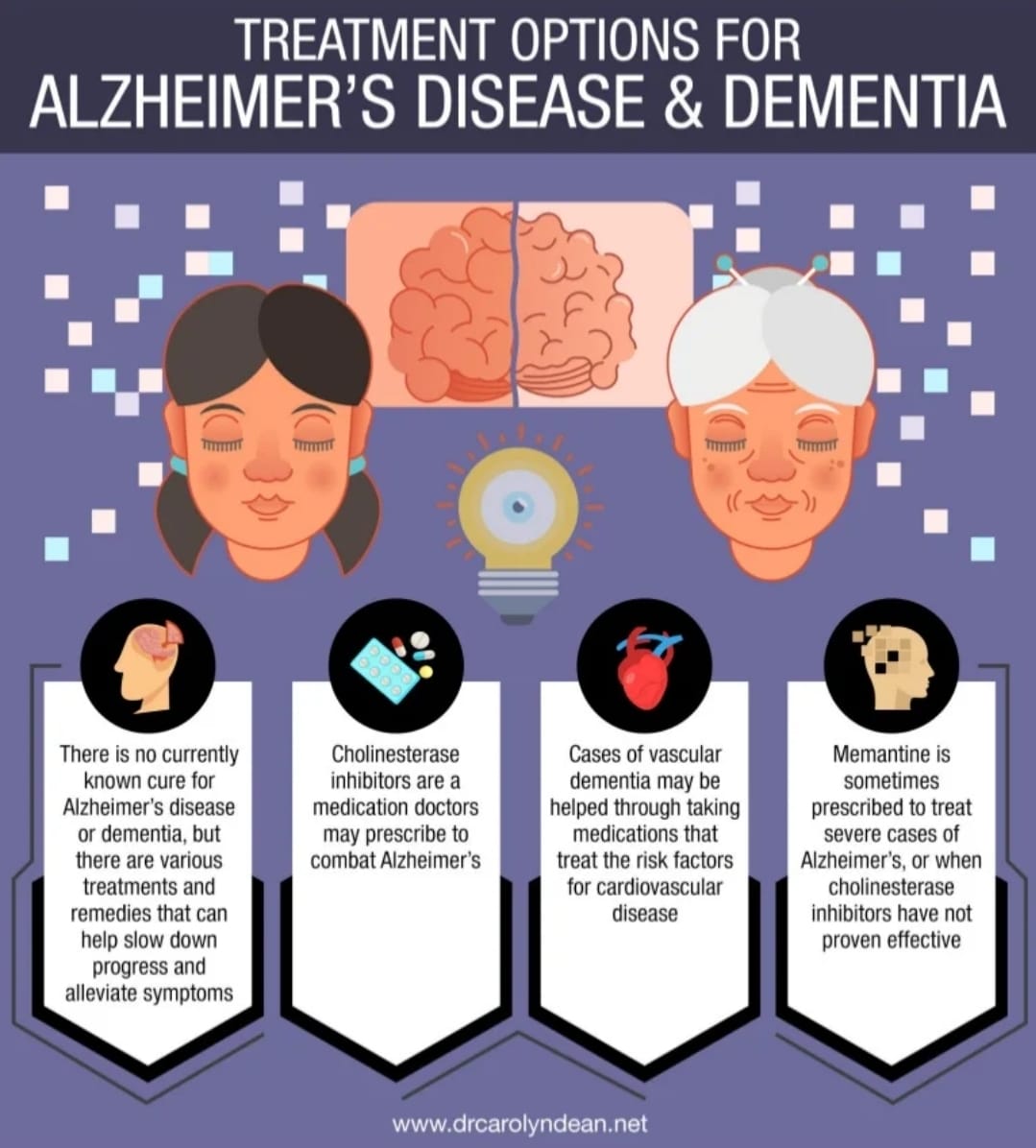
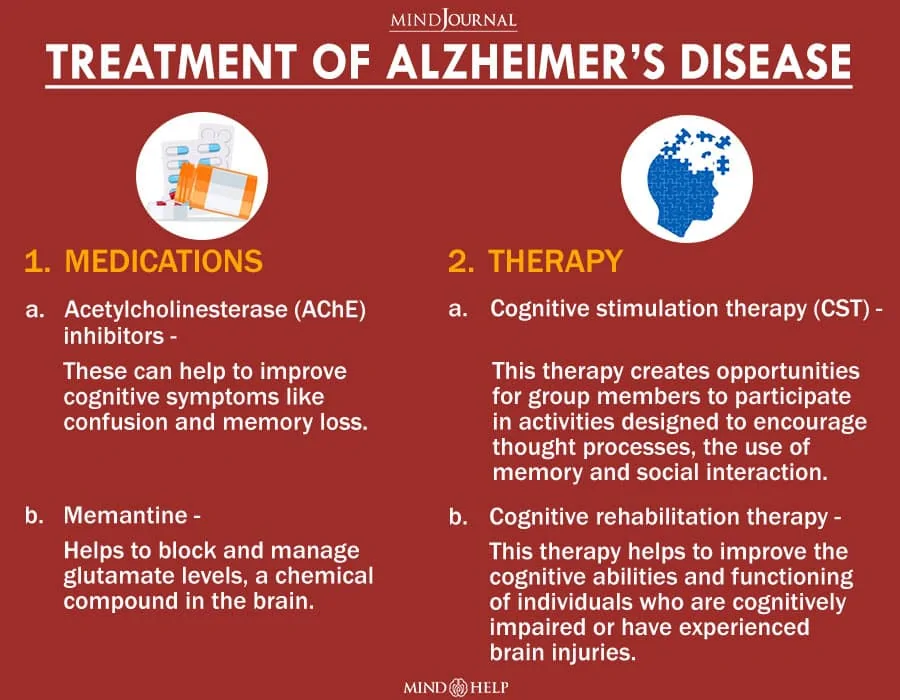
Treatment and
Interventions
While there is no
cure for Alzheimer's disease, there are medications that can temporarily
alleviate symptoms. Non-pharmacological approaches, such as creating a
structured environment and engaging in cognitive exercises, can also help
manage the condition.
Cholinesterase Inhibitors: These medications, including donepezil, rivastigmine, and galantamine, are often prescribed to manage cognitive symptoms in Alzheimer's disease. They work by increasing the levels of acetylcholine, a neurotransmitter involved in memory and learning. A meta-analysis by Birks (2006) found that cholinesterase inhibitors provide modest cognitive benefits in Alzheimer's patients, especially in the early and moderate stages.
Memantine: Memantine is another medication used to manage Alzheimer's symptoms. It regulates glutamate, a neurotransmitter involved in learning and memory, and is typically prescribed for moderate to severe stages of the disease. A study by Tariot et al. (2004) published in Alzheimer Disease and Associated Disorders demonstrated that memantine can help stabilize or slow cognitive decline in moderate to severe Alzheimer's.
Lifestyle and Non-Pharmacological Interventions
Cognitive Stimulation: Engagement in mentally stimulating activities, such as puzzles, games, and learning new skills, can help maintain cognitive function and slow decline. A study by Valenzuela and Sachdev (2006) in The Lancet Neurology suggests that cognitive engagement may reduce the risk of dementia and improve cognitive outcomes in older adults.
Physical Exercise: Regular physical activity has been linked to cognitive benefits and may reduce the risk of cognitive decline. Studies like Norton et al. (2012) in Alzheimer's & Dementia indicate that exercise interventions can improve cognitive function in older adults.
Nutrition: A balanced diet rich in antioxidants and omega-3 fatty acids may support brain health. The Mediterranean diet, which emphasizes fruits, vegetables, and healthy fats, has been associated with a reduced risk of Alzheimer's disease. Research by Scarmeas et al. (2009) in Archives of Neurology supports this link.
Social Engagement: Maintaining social connections and participating in social activities can help combat feelings of loneliness and isolation. A study by Wilson et al. (2002) in Archives of Neurology suggests that social engagement is associated with a reduced risk of Alzheimer's disease.
Preventing
Alzheimer's
While there is no
guaranteed way to prevent Alzheimer's disease, there is growing evidence to
suggest that certain lifestyle choices and risk factor management may help
reduce the risk of developing this condition.
1. Stay Physically
Active
Engaging in regular physical activity has been associated with a lower risk of cognitive decline. A study by Hamer and Chida (2009) in the journal Psychological Medicine found that physical activity is linked to a reduced risk of cognitive impairment.
2. Follow a
Heart-Healthy Diet
The Mediterranean diet, which emphasizes fruits, vegetables, whole grains, and healthy fats like olive oil, has been associated with a lower risk of Alzheimer's disease. Research by Scarmeas et al. (2009) in the journal Archives of Neurology supports this connection.
3. Maintain a
Healthy Weight
Obesity in midlife has been linked to an increased risk of late-life dementia, including Alzheimer's disease. A study by Whitmer et al. (2005) in Neurology found that obesity in midlife is associated with a significantly higher risk of dementia later in life.
4. Keep Your Brain
Active
Engaging in mentally stimulating activities, such as reading, puzzles, and learning new skills, may help reduce the risk of cognitive decline. A study by Wilson et al. (2002) in Archives of Neurology found that cognitive engagement is associated with a reduced risk of Alzheimer's disease.
5. Manage Chronic
Conditions
Managing chronic conditions like diabetes, hypertension, and high cholesterol through medication, lifestyle changes, and regular medical check-ups may help reduce the risk of Alzheimer's disease. A study by Qiu et al. (2011) in The Lancet Neurology suggests that midlife diabetes is associated with an increased risk of late-life dementia.
6. Social
Engagement
Staying socially active and maintaining strong social connections may have a protective effect against cognitive decline. A study by Fratiglioni et al. (2004) in The Lancet Neurology found that social engagement is associated with a reduced risk of dementia.
7. Get Quality
Sleep
Poor sleep patterns and sleep disorders have been linked to a higher risk of cognitive decline. Research by Yaffe et al. (2011) in Archives of Neurology suggests that sleep disturbances are associated with an increased risk of dementia.
It's important to
note that while these lifestyle factors may help reduce the risk of Alzheimer's
disease, they do not guarantee prevention. Additionally, genetics also play a
role in Alzheimer's risk, and some factors may be beyond an individual's
control. Nevertheless, adopting a healthy lifestyle that includes these
preventive measures can contribute to overall well-being and brain health.
Individuals concerned about Alzheimer's risk should consult with healthcare
professionals for personalized guidance and risk assessment.
Conclusion
In conclusion, Alzheimer's disease is a complex condition that affects not only the individual diagnosed but also their entire support network. Early recognition, diagnosis, and compassionate care are paramount. While there is currently no cure, ongoing research offers hope for future advancements in Alzheimer's treatment and management. By understanding the causes, symptoms, and preventive care strategies outlined in this blog post, individuals and families can better navigate the journey ahead.










Comments
Post a Comment