Protecting Your Vascular Health: Understanding Peripheral Vascular Disease
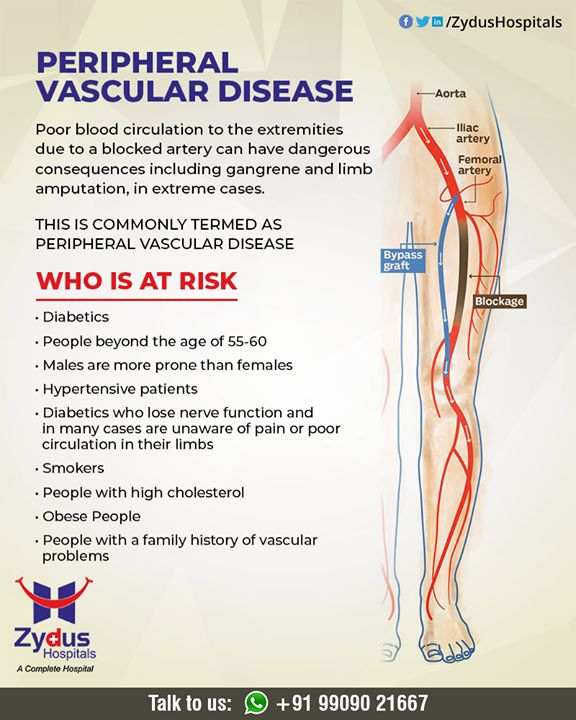
What is Peripheral Vascular Disease (PVD)?
Peripheral vascular
disease refers to a group of disorders that affect the blood vessels beyond the
heart and brain. The most common form of PVD is peripheral artery disease
(PAD), which primarily affects the arteries supplying blood to the legs and
feet. However, PVD can also involve other blood vessels, such as those in the
arms, stomach, and kidneys.
In healthy
individuals, arteries carry oxygen-rich blood from the heart to various parts
of the body, delivering essential nutrients and oxygen to cells and tissues.
However, in individuals with PVD, the arteries become narrowed or blocked due
to the buildup of fatty deposits, cholesterol, and other substances on the
walls of the blood vessels. This process, known as atherosclerosis, restricts
blood flow to the affected areas, leading to a range of symptoms and
complications.
Atherosclerosis
begins with damage to the inner lining of the arteries, often caused by factors
such as smoking, high blood pressure, high cholesterol, diabetes, obesity, and
physical inactivity. In response to this damage, the body initiates an inflammatory
process, leading to the accumulation of plaque within the arterial walls. Over
time, the plaque hardens and narrows the arteries, reducing blood flow to the
tissues and organs they supply.
Causes of Peripheral Vascular Disease
The primary cause of peripheral vascular disease is atherosclerosis, a condition characterized by the buildup of fatty deposits, cholesterol, and other substances on the walls of the arteries. Over time, these deposits can harden and narrow the arteries, reducing blood flow to the affected areas.
Other factors that contribute to the development of PVD include:
Smoking: Tobacco
use is a significant risk factor for PVD as it damages the lining of the
arteries and promotes the buildup of plaque.
High Blood
Pressure: Hypertension can strain the arteries, making them more susceptible to
damage and atherosclerosis.
High Cholesterol:
Elevated levels of LDL cholesterol ("bad" cholesterol) can contribute
to the formation of plaque in the arteries.
Diabetes:
Individuals with diabetes are at higher risk of developing PVD due to damage to
the blood vessels caused by high blood sugar levels.
Obesity: Being
overweight or obese increases the risk of developing atherosclerosis and PVD.
Physical
Inactivity: Lack of regular exercise can contribute to poor circulation and
increase the risk of PVD.
Symptoms of Peripheral Vascular Disease
PVD often develops gradually over time, with symptoms worsening as the condition progresses. Recognizing the signs of PVD is essential for early detection and intervention to prevent complications and improve outcomes.
Gradual Onset of
Symptoms
PVD typically
presents with a gradual onset of symptoms, which may initially be mild or
intermittent. Many individuals with PVD may not experience noticeable symptoms
in the early stages of the disease. However, as arterial blockages worsen and
blood flow becomes increasingly compromised, symptoms may become more
pronounced and persistent.
Common Signs and Symptoms
The most common
signs and symptoms of PVD include:
Pain or Cramping:
Pain, cramping, or discomfort in the legs, thighs, calves, or buttocks during
physical activity or exercise, a condition known as intermittent claudication.
This pain typically resolves with rest but may recur upon resuming activity.
Fatigue: Fatigue or
heaviness in the legs, especially after walking or standing for prolonged
periods. Individuals with PVD may experience decreased endurance and stamina
due to reduced blood flow to the lower extremities.
Weakness: Weakness
or numbness in the legs, feet, or toes, particularly during exertion or when
elevating the legs. Muscle weakness may result from inadequate oxygen and
nutrient delivery to the affected tissues.
Progression of
Symptoms
As peripheral
vascular disease advances, symptoms may worsen and extend beyond intermittent
claudication. Individuals with advanced PVD may experience the following
progressive symptoms:
Persistent Pain:
Chronic or constant pain, numbness, tingling, or burning sensations in the legs
or feet, even at rest. This persistent pain may interfere with daily activities
and quality of life.
Non-healing Wounds:
Ulcers or sores on the legs, feet, or toes that do not heal or heal slowly.
Reduced blood flow impairs the body's ability to repair damaged tissues,
increasing the risk of infections and complications.
Changes in Skin
Appearance: Skin changes, such as pallor (pale skin), coolness, or
discoloration of the legs or feet. In severe cases, the skin may appear shiny,
thin, or fragile, with loss of hair and thickened toenails.
Gangrene: Tissue
death (gangrene) in the affected limbs due to severe ischemia (lack of blood
flow). Gangrene is a serious complication of advanced PVD and may necessitate
amputation if left untreated.
Diagnosis of Peripheral Vascular Disease
Diagnosing
peripheral vascular disease (PVD) typically involves a comprehensive evaluation
of medical history, physical examination, and diagnostic tests to assess blood
flow and identify arterial blockages. Early detection and diagnosis are essential
for implementing appropriate treatment strategies and preventing complications
associated with PVD.
Medical History and
Physical Examination
Healthcare
providers will begin by conducting a thorough medical history assessment to
identify risk factors and symptoms suggestive of PVD. A detailed history may
include questions about lifestyle habits, such as smoking, physical activity
level, and presence of comorbid conditions like diabetes or hypertension.
During the physical examination, the healthcare provider will assess pulses in
the extremities, examine skin integrity, and evaluate for signs of arterial
insufficiency, such as pallor, coolness, or non-healing wounds.
Ankle-Brachial Index (ABI)
The ankle-brachial index (ABI) is a non-invasive test used to assess blood flow and detect arterial blockages in the lower extremities. During the ABI test, blood pressure measurements are obtained using a Doppler ultrasound device at the ankle and compared to blood pressure measurements in the arm. A lower ABI value indicates reduced blood flow to the legs and may suggest the presence of PVD.
Ultrasound Imaging
Doppler ultrasound
imaging is commonly used to evaluate blood flow and detect arterial narrowing
or blockages in the lower extremities. Ultrasound technology allows healthcare
providers to visualize the arteries and assess the severity of vascular disease.
Duplex ultrasound combines traditional ultrasound with Doppler technology to
provide detailed images of blood flow patterns and identify areas of stenosis
or occlusion.
Angiography
Angiography is an invasive diagnostic procedure used to visualize the blood vessels and identify blockages or narrowing. During angiography, a contrast dye is injected into the arteries, and X-ray imaging is performed to capture detailed images of the vascular system. Angiography can help pinpoint the location and severity of arterial disease and guide treatment decisions, such as angioplasty or stent placement.
Other Diagnostic
Tests
Additional
diagnostic tests may be employed to assess vascular health and identify
underlying conditions contributing to PVD. These tests may include magnetic
resonance angiography (MRA), computed tomography angiography (CTA), or arterial
pressure measurements.
Early and accurate
diagnosis of peripheral vascular disease is essential for initiating
appropriate treatment interventions and preventing complications such as limb
ischemia and tissue loss. Individuals experiencing symptoms suggestive of PVD
should undergo a thorough evaluation by a healthcare professional to determine
the underlying cause and develop a personalized treatment plan.
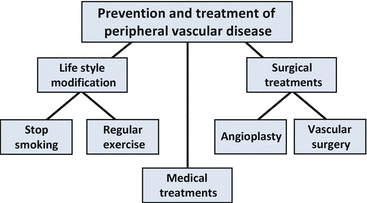
Treatment of
Peripheral Vascular Disease
The management of
peripheral vascular disease (PVD) aims to relieve symptoms, improve blood flow
to the affected limbs, and reduce the risk of complications such as limb
ischemia and tissue loss. Treatment strategies may vary depending on the
severity of the disease, underlying causes, and individual patient factors. A
multidisciplinary approach involving lifestyle modifications, medication
therapy, minimally invasive procedures, and surgical interventions may be
recommended to optimize outcomes for patients with PVD.
Lifestyle
Modifications
Lifestyle changes
play a crucial role in managing PVD and reducing cardiovascular risk factors.
Healthcare providers may recommend lifestyle modifications, including smoking
cessation, regular exercise, weight management, and a heart-healthy diet low in
saturated fats and cholesterol. Physical activity can improve circulation,
lower blood pressure, and enhance overall cardiovascular health.
Medication Therapy
Pharmacological
treatment options may be prescribed to manage symptoms, prevent complications,
and reduce the progression of PVD. Medications commonly used in the treatment
of PVD include:
Antiplatelet
Agents: Aspirin or clopidogrel may be prescribed to reduce the risk of blood
clot formation and improve blood flow.
Cholesterol-Lowering
Medications: Statins may be prescribed to lower cholesterol levels and stabilize
atherosclerotic plaques, reducing the risk of cardiovascular events.
Blood Pressure
Medications: Antihypertensive medications may be recommended to control blood
pressure and minimize the risk of hypertension-related complications.
Minimally Invasive
Procedures
Minimally invasive
procedures, such as angioplasty and stenting, may be performed to restore blood
flow to the affected arteries and alleviate symptoms of PVD. During
angioplasty, a catheter with a balloon at its tip is inserted into the narrowed
artery and inflated to widen the vessel and improve blood flow. In some cases,
a stent—a small mesh tube—is inserted to help keep the artery open and prevent
re-narrowing.
Surgical
Interventions
In severe cases of
PVD or when minimally invasive procedures are not effective, surgical
interventions may be necessary to bypass or remove blockages in the arteries.
Surgical options for PVD may include:
Peripheral Artery
Bypass Surgery: During bypass surgery, a healthy blood vessel (graft) is used
to reroute blood flow around the blocked artery, restoring blood flow to the
affected limb.
Endarterectomy:
Endarterectomy involves the surgical removal of plaque buildup from the inner
lining of the artery, improving blood flow and reducing the risk of thrombosis.
Wound Care and Limb
Preservation
For individuals
with advanced PVD and chronic wounds or tissue loss (ulcers), specialized wound
care and limb preservation strategies may be implemented to promote healing,
prevent infection, and preserve limb function. This may involve the use of
wound dressings, debridement procedures, and offloading devices to reduce
pressure on affected areas.
Source:
Dhalla, N.S., Camargo, R.O., Elimban, V., Dhadial, R.S., Xu, YJ. (2017). Role of Skeletal Muscle Angiogenesis in Peripheral Artery Disease. In: Mehta, J., Mathur, P., Dhalla, N. (eds) Biochemical Basis and Therapeutic Implications of Angiogenesis. Advances in Biochemistry in Health and Disease, vol 6. Springer, Cham. https://doi.org/10.1007/978-3-319-61115-0_23Prevention of Peripheral Vascular Disease
While some risk
factors for PVD, such as age and family history,
cannot be modified, several lifestyle modifications and preventive measures can
help reduce the risk of developing PVD and its associated complications. Adopting
a heart-healthy lifestyle and managing underlying cardiovascular risk factors
are key strategies for preventing the progression of PVD and preserving
vascular health. Below are some important preventive measures individuals can
take to reduce their risk of PVD:
Smoking Cessation
Smoking is a major
risk factor for the development and progression of PVD. Tobacco smoke damages
blood vessels, accelerates the formation of atherosclerotic plaques, and
impairs circulation. Quitting smoking is one of the most effective ways to
reduce the risk of PVD and improve overall cardiovascular health. Smoking
cessation programs, counseling, and nicotine replacement therapies may be
helpful for individuals trying to quit smoking.
Regular Exercise
Engaging in regular
physical activity is essential for maintaining cardiovascular health and
reducing the risk of PVD. Regular exercise helps improve blood flow, lower
blood pressure, control weight, and strengthen the heart and blood vessels. Aim
for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes
of vigorous-intensity aerobic exercise per week, as recommended by health
guidelines. Activities such as walking, swimming, cycling, and jogging can help
improve circulation and lower the risk of PVD.
Healthy Diet
Following a
heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and
healthy fats can help prevent the development of PVD and reduce cardiovascular
risk factors. Choose foods low in saturated fats, trans fats, cholesterol, and
sodium, and limit the consumption of processed and high-calorie foods. A diet
high in fiber, antioxidants, and omega-3 fatty acids can help lower cholesterol
levels, control blood sugar, and promote vascular health.
Maintain a Healthy
Weight
Excess body weight
and obesity are significant risk factors for PVD and other cardiovascular
conditions. Maintaining a healthy weight through a balanced diet and regular
exercise can help reduce the strain on the heart and blood vessels, improve
circulation, and lower the risk of developing PVD. Aim for a body mass index
(BMI) within the normal range (18.5 to 24.9 kg/m²) to lower your risk of
obesity-related complications.
Control Blood
Pressure and Cholesterol
High blood pressure
(hypertension) and elevated cholesterol levels are important risk factors for
PVD. Monitoring blood pressure and cholesterol levels regularly and taking
steps to keep them within target ranges can help prevent the progression of PVD
and reduce the risk of cardiovascular events. Follow healthcare provider
recommendations for blood pressure management, cholesterol-lowering medications
(if prescribed), and lifestyle modifications to control these risk factors
effectively.
Manage Diabetes
Individuals with
diabetes are at increased risk of developing PVD due to the damaging effects of
high blood sugar on blood vessels and nerves. Proper management of diabetes
through medication, blood sugar monitoring, healthy eating, regular exercise,
and routine medical check-ups is essential for preventing complications and
preserving vascular health. Follow healthcare provider recommendations for
diabetes management and seek support from diabetes educators and healthcare
professionals as needed.
Regular Health
Check-ups
Regular health
screenings and preventive healthcare visits can help identify and manage risk
factors for PVD and other cardiovascular conditions early. Routine screenings
for blood pressure, cholesterol, blood sugar, and other cardiovascular risk
factors can help detect abnormalities and guide appropriate interventions to
prevent the progression of PVD. Discuss your individual risk factors, lifestyle
habits, and preventive strategies with your healthcare provider to develop a
personalized prevention plan tailored to your needs.
By adopting a
heart-healthy lifestyle, managing cardiovascular risk factors, and seeking
regular medical care, individuals can significantly reduce their risk of
developing peripheral vascular disease (PVD) and maintain optimal vascular
health throughout life. Making informed lifestyle choices and adhering to
preventive measures are essential for protecting against PVD and reducing the
burden of cardiovascular disease in the population.
Conclusion
Peripheral vascular
disease (PVD) poses significant risks to vascular health and overall
well-being, particularly among individuals with underlying cardiovascular risk
factors. By understanding the causes, symptoms, diagnosis, treatment options,
and preventive measures associated with PVD, individuals can take proactive
steps to preserve vascular health and reduce the risk of complications.
Embracing a heart-healthy lifestyle, including regular exercise, healthy
eating, smoking cessation, and proactive management of cardiovascular risk
factors, is crucial for preventing the development and progression of PVD.
Through awareness, education, and preventive action, individuals can safeguard
their vascular health and enhance their quality of life.





Comments
Post a Comment