Meaningful Connections: Harnessing Active Listening and Empathy with Seniors
In the world of health and community care, building
meaningful connections with seniors is paramount. Active listening is a
powerful tool that can foster trust, understanding, and a sense of being truly
heard. It's more than just sitting quietly while someone speaks; it's a conscious
effort to engage with the speaker's message on a deeper level. Active
listening, paired with genuine empathy, offers a powerful way to bridge this
gap.
For seniors, effective communication isn't just about exchanging information—it's about connection, validation, and understanding. Whether it's a conversation between family members, caregivers, or healthcare professionals, actively listening with empathy can transform a simple dialogue into a meaningful exchange. This practice not only honours the life stories and experiences of seniors but also enhances their emotional well-being, making them feel respected and valued.
In this blog post, we will explore the importance of active
listening with empathy in fostering deeper, more meaningful connections with
seniors. We'll delve into practical strategies for implementing these skills
and discuss the profound impact they can have on the quality of relationships
and the lives of the seniors we interact with.
What is Active Listening?
Active listening is more than just hearing the words someone says, it’s an engaged and deliberate process of paying full attention to the speaker, understanding their message, and responding thoughtfully. In healthcare and community care settings, active listening is a critical communication skill that enables providers to gather important information, build trust, and create a supportive environment for patients, particularly seniors.
Key components of active listening include:
1. Full Attention: is the cornerstone of active listening, particularly in the context of communicating with seniors. It involves being completely present in the moment, giving the speaker your undivided focus, and actively engaging in the conversation. This level of attention is critical in healthcare and caregiving environments, where the quality of communication can directly impact the well-being and emotional health of seniors.
Minimizing Distractions
In today’s fast-paced world, distractions are
everywhere—from the buzzing of a mobile phone to the hustle and bustle of a
busy clinic or care facility. For seniors, who may already struggle with
hearing, cognitive processing, or the effects of isolation, these distractions
can make it even more difficult to feel heard and understood. Healthcare
providers and caregivers can minimize distractions by:
·
Creating
a Quiet Environment:
Whenever possible, hold conversations in a quiet, private space, free from
background noise or interruptions. This helps the senior focus on the
conversation and feel more at ease.
·
Silencing
Devices:
Putting phones on silent mode and avoiding the use of electronic devices during
the conversation signals to the senior that they have your full attention.
·
Managing
Time Effectively:
Ensure that the time set aside for conversations is sufficient and not rushed.
If the senior perceives that you are in a hurry, they may feel their concerns
are not important.
Asking Open-Ended Questions
Open-ended questions are inquiries
that cannot be answered with a one-word response. They are designed to promote
conversation and provide the senior with the opportunity to share their
thoughts, experiences, and emotions more freely.
Instead of yes/no questions, active
listeners use open-ended questions to encourage deeper conversation. These
questions often begin with words like "how," "what,"
"why," "tell me about," or "describe." For
instance, asking "Can you tell me more about how you've been feeling
lately?" invites the senior to share more about their experiences,
feelings, and concerns.
Here are some practical tips for
healthcare and community care providers:
- Start with General Questions: Begin with broad, general questions to open the conversation and make the senior feel comfortable. For example, "Can you tell me about your day?" or "What’s been on your mind lately?" This sets a relaxed tone and allows the senior to share as much or as little as they like.
- Follow Up with Specifics: Once the conversation is flowing, use more specific open-ended questions to delve deeper into particular areas of concern. For example, if the senior mentions they’ve been feeling tired, you might ask, "What do you think might be causing your fatigue?" And if a senior mentions feeling lonely, you might ask, "What do you think would help you feel more connected to others?" or "Can you tell me more about when you started feeling this way?" This invites the senior to explore and share potential reasons or feelings related to their condition.
- Be Mindful of Tone and Body Language: When asking open-ended questions, your tone of voice and body language should convey genuine interest and concern. Speak slowly, maintain eye contact, and use a warm, inviting tone. This helps the senior feel safe and encouraged to open up.
- Give Them Time to Answer: Seniors may need more time to process the question and formulate their response. Be patient and give them the space they need to think and speak like using moments of silence. Avoid rushing them or interrupting, as this can make them feel pressured or less inclined to share. This demonstrates respect and understanding.
- Avoid Leading or Suggestive Questions: Ensure that your open-ended questions are neutral and non-judgmental, allowing the senior to express their true feelings without feeling pressured to respond in a certain way. For example, instead of asking, "Don’t you think it would be better if…?" you might ask, "What do you think about…?" This approach avoids leading them toward a specific answer and keeps the conversation open.
Examples of Open-Ended Questions in
Senior Care
Here are some examples of open-ended
questions that can be used in various scenarios when interacting with seniors:
·
Physical
Health:
"How have you been feeling physically over the past week?"
o
This
question invites the senior to discuss their overall health and any specific
symptoms or concerns they might have.
·
Emotional
Well-Being:
"What are some things that have been making you feel happy or content
lately?"
o
This
allows the senior to reflect on positive experiences or to share what might be
lacking in their emotional life.
·
Daily
Life and Routines:
"Can you walk me through what a typical day looks like for you?"
o
This
question encourages the senior to share details about their daily routines,
preferences, and any challenges they face.
·
Social
Connections:
"How have your relationships with friends and family been lately?"
o
This
opens the door for seniors to talk about their social life, potentially revealing
feelings of loneliness or isolation that might not be otherwise addressed.
·
Care
Experience:
"What are your thoughts on the care you’re receiving? Is there anything
you’d like to change?"
o
This
question invites feedback on the care they’re receiving, helping caregivers
identify areas for improvement.
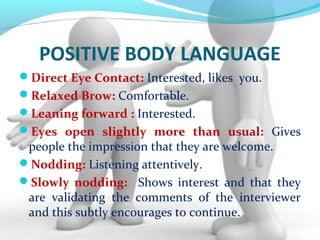
Engaging Body Language
Non-verbal cues play a significant role in communication, often conveying as much, if not more, than words alone. Seniors, particularly those who may struggle with hearing or cognitive decline, often rely on visual cues to interpret the emotions and intentions behind words. Therefore, the way a caregiver or healthcare provider uses body language is crucial in demonstrating full attention.
Key aspects of engaging body language include:
·
Maintaining
Eye Contact:
Eye contact is a powerful way to convey interest and concern. For seniors, it
reassures them that they are the focus of the conversation. However, be mindful
that eye contact should be gentle and non-intimidating.
·
Open
Posture:
Facing the senior directly, with uncrossed arms and an open stance, indicates
that you are receptive and ready to listen. Leaning slightly forward can also
show engagement and interest.
·
Nods
and Small Gestures:
Nodding your head or using small affirming gestures, such as a slight smile or
a soft “mm-hmm,” can encourage the senior to continue speaking and show that
you are following along.
Active Mental Engagement
Full attention isn’t just about being physically present;
it also requires mental engagement. This means focusing your thoughts entirely
on what the senior is saying, rather than thinking about your next task or how
you will respond. Mental engagement allows you to better understand the nuances
of the conversation, such as the underlying emotions or concerns the senior
might be expressing indirectly. To achieve active mental engagement:
·
Listen
to Understand, Not to Respond: Focus on truly understanding the senior’s perspective and
emotions, rather than planning your response while they are still speaking.
This helps ensure that your feedback or comments are relevant and
compassionate.
·
Reflect
on the Speaker’s Words:
Internally summarizing or reflecting on what the senior has said can help you
stay focused. This practice also prepares you to paraphrase their statements if
clarification is needed.
·
Acknowledge
Emotional Cues:
Pay attention to any emotional undertones in the senior’s voice or choice of
words. This can provide valuable insight into how they are feeling and what
might be important to them at the moment.
·
Avoiding Interruptions: Active listeners
resist the urge to interrupt or rush the speaker. This is crucial when
communicating with seniors, who may take longer to express their thoughts due
to age-related cognitive or speech challenges. Allowing them to speak at their
own pace shows respect and patience.
2. Reflective Listening: is a vital
component of active listening, especially in interactions with seniors. It
involves carefully hearing what the speaker is saying and then reflecting back,
or paraphrasing, that message to confirm understanding. This practice helps
ensure that communication is clear and that the listener accurately comprehends
the speaker's thoughts, feelings, and concerns.
Reflective listening is especially important in healthcare and community
care settings, where effective communication can directly impact a senior’s
well-being, care outcomes, and overall satisfaction with the services they
receive.
At its core, reflective listening is about echoing back
what the speaker has said, not just the words, but also the underlying feelings
and meanings. This approach helps in several key ways:
·
Clarifying
Communication:
By reflecting back what the senior has said, you help ensure that there is no
misunderstanding or miscommunication. For example, if a senior says, "I’ve
been feeling very tired lately," a reflective response could be, "It
sounds like you’ve been feeling unusually fatigued. Is that right?" This
confirms that you understood their message correctly.
·
Validating
Emotions:
Reflective listening also involves acknowledging the emotions behind the words.
For instance, if a senior expresses frustration about their physical
limitations, reflecting that emotion shows empathy and understanding, which can
be deeply comforting.
·
Encouraging
Further Expression:
Reflective listening can encourage seniors to share more about their
experiences and feelings. When they feel that their concerns are being
accurately understood and validated, they may feel more comfortable opening up
about deeper issues.
The Mechanics of Reflective Listening
Reflective listening can be broken down into a few key
steps that healthcare and community care providers can practice:
·
Listen
for Content and Emotion:
When a senior speaks, pay attention not just to the content of their words, but
also to the emotions they might be conveying. For example, if a senior says, “I
don’t like it when my routine is changed,” the underlying emotion might be
anxiety or discomfort with unpredictability.
·
Paraphrase
and Reflect:
After listening, restate what you’ve heard in your own words. For example, you
might say, “It seems like changes to your routine make you feel unsettled. Is
that how you’re feeling?” This shows that you’re not just repeating their words
but also interpreting and acknowledging their emotional experience.
·
Ask
for Confirmation:
After reflecting back what you’ve heard, ask the senior if your reflection is
accurate. This invites them to clarify or expand on their original statement,
which can lead to a deeper understanding. For example, “Am I understanding you
correctly? Does this change in routine make you anxious?”
·
Avoid
Judgement:
Reflective listening is about understanding and supporting, not judging or
advising. Even if you might disagree with the senior’s perspective or feelings,
the goal is to validate their experience and make them feel heard, rather than
offering solutions or criticisms right away.
Practical Examples of Reflective Listening in Action
Reflective listening can be
applied in a variety of situations in healthcare and community care settings.
Here are a few examples:
Example 1: Health Concerns
o Senior:
“I’ve been feeling a lot of pain in my joints lately, and it’s really been
getting me down.”
o Reflective
Response: “It sounds like the joint pain you’re experiencing is affecting your
mood and making it difficult for you. Is that correct?”
o This
reflection not only acknowledges the physical pain but also the emotional
impact it has on the senior.
Example 2: Change in Routine
o Senior:
“I don’t like it when they change my mealtime. It makes everything feel out of
order.”
o Reflective
Response: “You’re saying that changes to your mealtime make you feel unsettled
and disrupt your routine. Is that what you mean?”
o This
reflection shows an understanding of the senior’s need for consistency and
order, which is often important for their sense of control and comfort.
Example 3: Feelings of
Loneliness
o Senior:
“I don’t see my family as much as I used to, and I feel very alone.”
o Reflective
Response: “It sounds like you’re feeling lonely because you don’t get to see
your family as often as you’d like. Is that right?”
o This
reflective response acknowledges the senior’s emotional state and invites
further discussion, which could lead to identifying ways to help them feel more
connected.
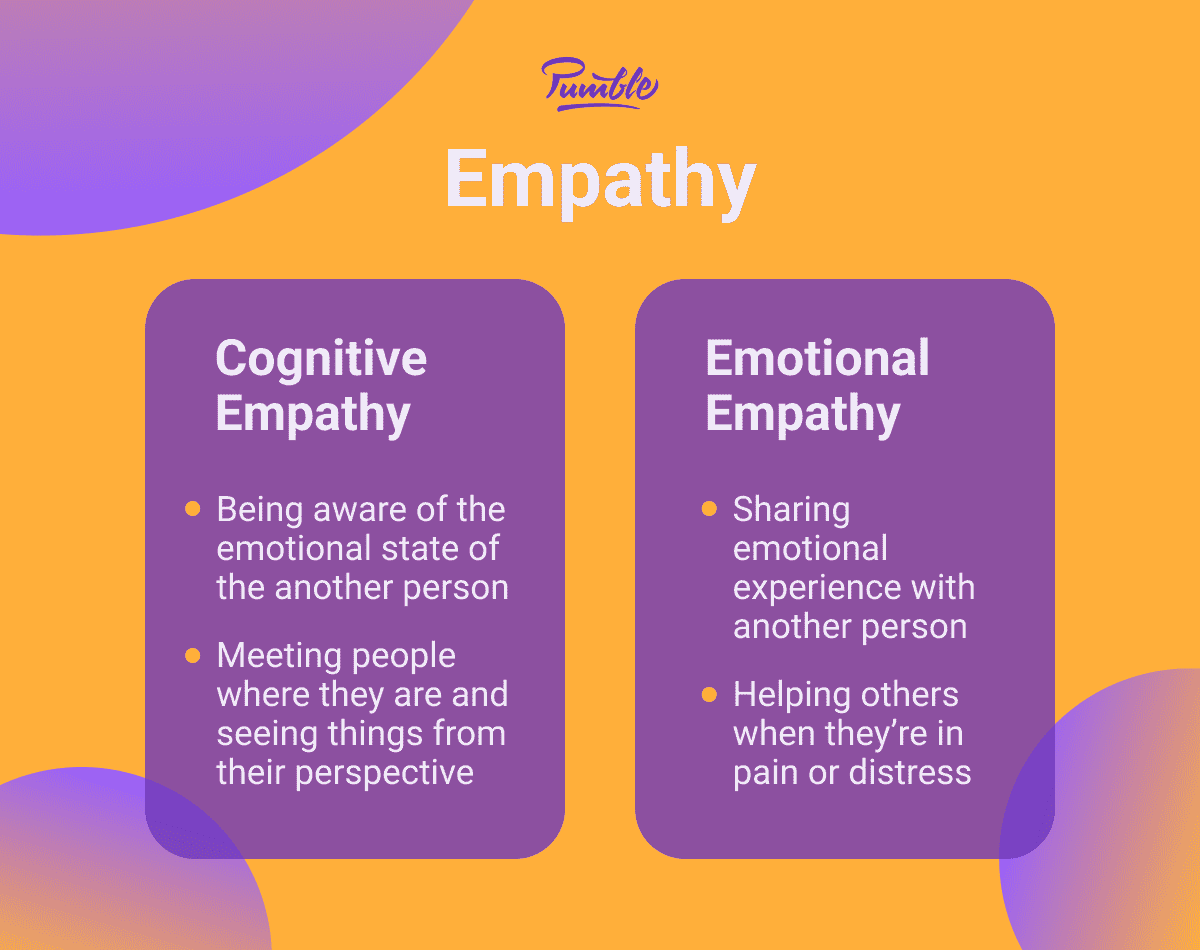
What is Empathy?
Empathy is the ability to understand and share the feelings of another person. In the context of healthcare and community care, empathy goes beyond acknowledging a patient’s emotions; it involves genuinely connecting with those emotions and responding in a way that validates the patient’s experience.
Key aspects of empathy include:
1.
Emotional Awareness: is a critical
component of empathy, particularly in the caregiving and healthcare settings
where understanding a senior's emotional state can significantly influence the
quality of care provided. Emotional awareness involves the ability to
recognize, understand, and appropriately respond to the emotions of others. For
healthcare providers and caregivers, developing emotional awareness means being
attuned not only to the overt expressions of emotion but also to the subtle
cues that seniors may give off, consciously or unconsciously. For
example, a senior might not explicitly state they’re feeling lonely, but their
tone of voice, facial expressions, or body language might reveal this. Emotional awareness refers to the ability to:
· Identify
and understand emotions: This involves recognizing not only what emotions
the senior might be experiencing (such as sadness, anxiety, frustration, or
joy) but also understanding why they might be feeling that way.
· Perceive
emotional cues: Seniors may express their emotions through various
channels, including facial expressions, tone of voice, body language, and the
content of their speech. Emotional awareness requires being sensitive to these
cues, even when they are subtle or contradictory to what is being said.
· Manage
your own emotions: A key aspect of emotional awareness is the ability to
regulate your own emotional responses. This includes maintaining a calm and
supportive demeanor, even when faced with challenging emotional situations,
ensuring that your emotions do not negatively impact the interaction.
Healthcare and community care providers can enhance their emotional awareness by focusing on several key strategies:
·
Active Observation: Pay close attention
to the senior’s non-verbal cues, such as facial expressions, body language, and
tone of voice. For example, a senior who says they are "fine" but
avoids eye contact and speaks in a low, hesitant tone might be feeling
depressed or anxious.
·
Listening Beyond Words: Emotional
awareness requires listening not just to what is being said, but also to how it
is being said. The emotions conveyed through tone, pace, and volume of speech
can provide important clues about how the senior is really feeling. For
example, a senior who speaks quickly and with a raised voice may be expressing
anger or frustration, even if their words do not explicitly state this.
·
Asking Reflective Questions: To better
understand the senior’s emotional state, ask questions that encourage them to
explore their feelings. For example, "How do you feel about the changes in
your health recently?" or "It seems like you might be feeling
overwhelmed. Would you like to talk more about what’s on your mind?"
·
Self-Reflection: Developing emotional
awareness also involves reflecting on your own emotional responses and how they
might affect your interactions with seniors. For instance, if you notice that
you are feeling frustrated, take a moment to understand why, and consider how
you can manage that emotion to avoid it impacting your care.
· Empathetic Validation: Once you have identified the senior’s emotional state, it’s important to validate their feelings, even if they are difficult or uncomfortable. For example, if a senior expresses fear about their health, an empathetic response might be, "I can understand why you might feel scared. It’s completely normal to feel that way, and I’m here to support you through this."
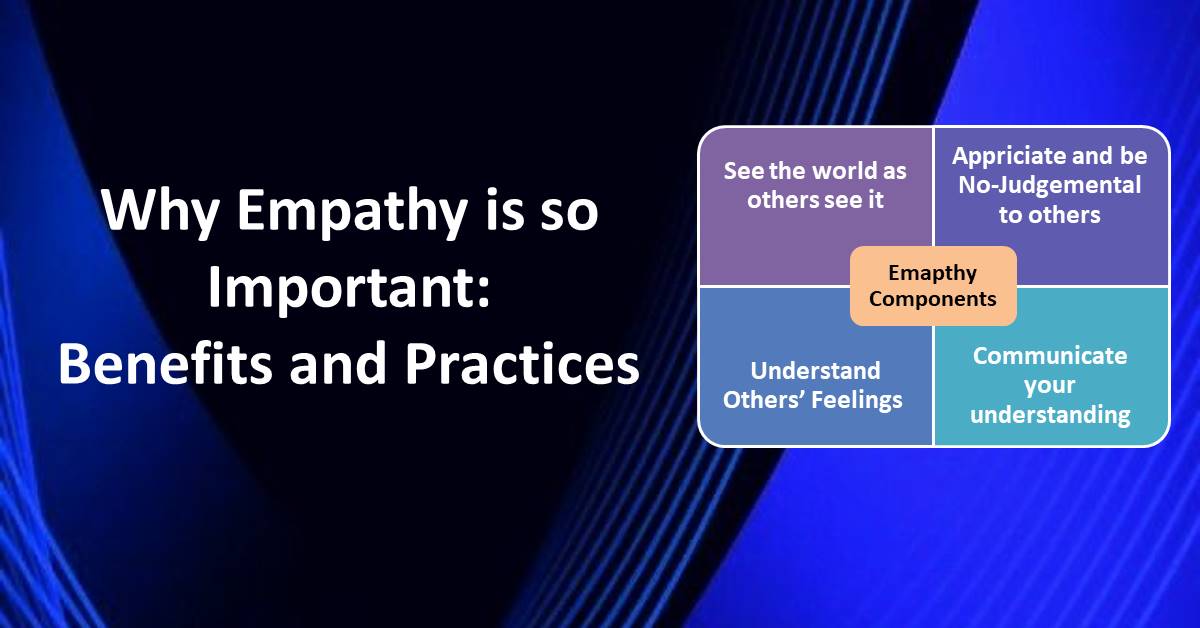
- Perspective-Taking: Empathy involves putting yourself in the other person’s shoes—imagining what it’s like to be in their situation by considering their experiences, emotions and thoughts from their perspective. For seniors, who may be facing issues such as declining health, loss of independence, or bereavement, this perspective-taking helps providers understand the emotional weight of these experiences. For healthcare and community care providers working with seniors, perspective taking is essential for delivering care that is truly empathetic, respectful, and responsive to the unique needs and challenges faced by older adults
Perspective taking is the cognitive process of:
·
Understanding someone else's viewpoint:
This involves trying to see the world as the other person sees it, including
their thoughts, feelings, and motivations.
·
Recognizing their experiences and history:
For seniors, this often means acknowledging the rich tapestry of their past
experiences, which shapes how they view the present.
·
Anticipating their needs and concerns: By
understanding a senior’s perspective, caregivers can better anticipate their
needs, whether emotional, physical, or social.
Healthcare and community care
providers can enhance their perspective taking by focusing on several key
strategies:
- Engage
in Active Listening: To understand a senior’s perspective, start by
truly listening to what they are saying. This means paying attention not
just to their words, but also to their tone, body language, and underlying
emotions. For example, if a senior expresses frustration with a new
routine, try to understand what it is about the change that bothers them.
Is it a loss of independence? A feeling of being rushed?
- Ask
Clarifying Questions: When trying to understand a senior’s
perspective, it’s important to ask questions that help you see things from
their viewpoint. For example, "Can you tell me more about how you
feel when we go through this daily routine?" or "What’s most
important to you in this situation?" These questions invite the
senior to share more about their thoughts and feelings, providing you with
greater insight.
- Consider
Their Life History: A senior’s perspective is often shaped by their
past experiences, including their career, family life, and significant
events. Understanding this history can help you better understand their
current perspective. For instance, a senior who was a caregiver for others
may find it particularly difficult to accept help now, due to their
ingrained sense of independence and responsibility.
- Put
Yourself in Their Shoes: Imagine how you might feel if you were in the
senior’s position. What would your concerns and priorities be? What
challenges might you face? For example, consider the emotional impact of
losing independence or dealing with chronic pain. By empathizing with
these challenges, you can better appreciate the senior’s perspective and
respond with greater sensitivity.
- Acknowledge
Their Feelings: Once you’ve taken the senior’s perspective into
account, it’s important to acknowledge their feelings and validate their
experiences. This might involve saying something like, "I can see how
this situation might be really frustrating for you," or "It
makes sense that you would feel anxious about this change." Such
validation helps the senior feel understood and respected.
- Be
Mindful of Generational Differences: Recognize that seniors may have
grown up in a different cultural or social context, which can influence
their values, beliefs, and expectations. Understanding these differences
can help you better navigate potential conflicts or misunderstandings. For
example, a senior who values self-sufficiency may resist certain types of
assistance, not because they don’t need it, but because accepting help
feels like a loss of dignity.
Here are some practical examples
of how perspective taking can be applied in caregiving situations:
- Example
1: Managing Resistance to Care
- A senior might resist using a walker because it makes them feel old and dependent. From the caregiver’s perspective, the walker is a safety necessity, but from the senior’s perspective, it represents a loss of independence. Understanding this, the caregiver can acknowledge the senior’s feelings and perhaps work together to find a more acceptable solution, like customizing the walker to make it feel more personal or explaining how it enhances their independence by preventing falls.
- Example
2: Navigating Emotional Conversations
- A
senior might express anger or frustration during a medical appointment,
which could be interpreted as being difficult or uncooperative. However,
by taking the senior’s perspective, the caregiver might realize that the
senior is actually scared or overwhelmed by the medical process. This
understanding can lead the caregiver to respond with more patience and
reassurance, rather than frustration.
- Example
3: Supporting Social Engagement
- A senior might withdraw from social activities, citing tiredness or lack of interest. While it’s easy to accept this at face value, taking their perspective might reveal deeper issues, such as fear of embarrassment due to memory loss or physical limitations. By understanding these concerns, a caregiver can offer alternative solutions, such as smaller group activities or more personalized social interactions that feel safer and more comfortable.
- Compassionate
Response: the act of transforming
empathy into meaningful action by responding in a way that
demonstrates genuine care, concern, and a desire to alleviate their
distress or enhance their well-being. This could be as simple as saying,
"I can see this is really difficult for you," or offering a
comforting gesture, like a hand on the shoulder. In healthcare, such responses can greatly
enhance the therapeutic relationship, making seniors feel understood and fostering
a sense of security that the care provided is both effective and humane.
A compassionate response
involves:
·
Recognizing and acknowledging the senior’s
emotions: This means being attuned to the emotional state of the senior,
whether they are feeling scared, lonely, frustrated, or happy.
·
Expressing empathy through words and actions:
Compassionate responses often begin with verbal acknowledgment of the senior’s
feelings, followed by actions that address their emotional and physical needs.
·
Taking appropriate actions to support the
senior: Compassion is demonstrated through actions that aim to alleviate
suffering, provide comfort, or enhance the senior’s well-being. This might
involve small gestures, like offering a comforting word, or more significant
interventions, like adjusting care plans to better meet their needs.
Healthcare and community care
providers can cultivate and demonstrate compassion through the following
strategies:
- Acknowledge Their Emotions: Start by acknowledging the senior’s emotions, no matter how minor they may seem. For example, if a senior expresses sadness or frustration, a simple but sincere acknowledgment like, "I can see that you’re feeling down today. Would you like to talk about it?" can make a significant difference.
- Offer Comfort and Reassurance: Sometimes, seniors just need to know that someone cares and is there for them. Offering comforting words or a gentle touch can provide reassurance. For example, saying, "I’m here for you, and we’ll get through this together," can help alleviate feelings of loneliness or fear.
- Take Action to Alleviate Distress: Compassionate responses often involve taking practical steps to address the senior’s needs. If a senior is feeling cold, offering a blanket or adjusting the room temperature shows that you are attentive to their comfort. If they are anxious about a medical procedure, explaining the process calmly and reassuring them can help ease their anxiety.
- Be Patient and Attentive: Compassionate care requires patience, especially when seniors are dealing with confusion, frustration, or physical limitations. Giving them time to express themselves without rushing or interrupting them demonstrates respect and understanding. It’s important to let them know that their feelings and experiences are important.
- Use Non-Verbal Communication: Compassionate responses aren’t always verbal. Non-verbal cues such as a warm smile, maintaining eye contact, or a gentle touch can convey compassion and understanding. For seniors who might have difficulty communicating verbally, these gestures can be especially meaningful.
Here are some practical examples
of how compassionate responses can be applied in caregiving situations:
- Example
1: Easing Anxiety Before a Procedure
- A
senior is visibly anxious about an upcoming medical procedure. The
caregiver notices this and responds compassionately by sitting with them,
explaining the procedure in simple, reassuring terms, and staying by
their side until the procedure begins. This shows the senior that they
are not alone and that their feelings are valid.
- Example
2: Providing Comfort During Loneliness
- A
senior who lives alone expresses feelings of loneliness. Instead of just
acknowledging these feelings, a compassionate response might involve the
caregiver arranging for regular check-ins, setting up video calls with
family members, or even spending extra time chatting with the senior to
help alleviate their loneliness.
- Example
3: Responding to Frustration
- A
senior is frustrated because they can no longer perform a task they used
to do independently. Instead of dismissing their frustration, a
compassionate response would involve acknowledging their feelings and
working together to find alternative ways to accomplish the task, perhaps
offering tools or modifications that make it easier for them to maintain
some level of independence.
- Non-Judgmental
Attitude: Empathy requires suspending judgment and accepting the
senior’s feelings and experiences as valid. This is especially important
when dealing with seniors who may express frustration, fear, or sadness.
Rather than trying to fix the situation or offer immediate solutions,
empathetic caregivers listen and validate these feelings, recognizing that
sometimes what the senior needs most is to be heard. In senior care, a non-judgmental
attitude helps create an environment where seniors feel safe to express
their true feelings and concerns, without fear of criticism or
misunderstanding. This is especially important as seniors may face a range
of challenges, from physical health issues to emotional struggles, that
require sensitive and respectful handling.
A non-judgmental attitude
involves:
·
Approaching every situation with an open
mind: This means suspending personal biases and preconceived notions to
fully understand the senior’s perspective.
·
Avoiding criticism or blame: Rather than
judging a senior’s feelings, behaviors, or decisions, caregivers focus on
understanding and supporting them.
· Accepting the senior’s emotions and experiences as valid: Even if the caregiver does not agree with or fully understand the senior’s perspective, they recognize that the senior’s feelings and experiences are real and important.
Healthcare and community care providers can cultivate and demonstrate a non-judgmental attitude through the following strategies:
·
Practice Active Listening Without
Interruption: When a senior is speaking, listen attentively without
interrupting or forming judgments. Allow them to express their thoughts and
feelings fully before responding. This shows respect and a willingness to
understand their perspective.
·
Recognize and Set Aside Personal Biases:
Everyone has biases, but it’s important to recognize them and consciously set
them aside when interacting with seniors. For example, if a senior expresses a
viewpoint that differs from your own, focus on understanding their perspective
rather than imposing your own beliefs.
·
Avoid Making Assumptions: Don’t assume
you know how a senior feels or what they need based on stereotypes or past
experiences with other seniors. Each person is unique, and their feelings and
experiences deserve to be understood on their own terms. For instance, if a
senior refuses a particular treatment, instead of assuming they are being
difficult, explore their reasons with an open mind.
·
Use Neutral and Supportive Language: The
language you use can significantly impact how a senior perceives your attitude.
Avoid language that could be perceived as critical or dismissive. For example,
instead of saying, "Why didn’t you take your medication?" which can
come across as accusatory, you might say, "Can you help me understand what
made it difficult for you to take your medication today?" This phrasing
invites dialogue without judgment.
·
Show Empathy and Understanding: Even if
you don’t agree with a senior’s choices or behavior, show empathy for their
situation. For example, if a senior is reluctant to use a walker, acknowledge
their feelings by saying, "I understand that using a walker might feel
frustrating or limiting. Let’s talk about how we can make it easier for
you."
·
Reflect on Your Own Reactions: After
interacting with a senior, take a moment to reflect on your own reactions. Were
there moments where you felt judgmental? How can you approach similar
situations differently in the future? This self-reflection helps you
continuously improve your non-judgmental approach.
Here are some practical examples of how a non-judgmental attitude can be applied in caregiving situations:
- Example 1: Responding to Resistance to Care
- A senior refuses to take their medication, expressing frustration with their health condition. Instead of reprimanding them or insisting they follow the treatment, a non-judgmental response would involve calmly discussing their concerns, listening to their reasons, and working together to find a solution that respects their autonomy while addressing their health needs.
- Example 2: Addressing Sensitive Topics
- A senior expresses regret or shame about a past decision or current situation, such as needing help with personal care. A non-judgmental response would involve acknowledging their feelings without making them feel worse. For example, saying, "It’s okay to feel that way. Many people find this difficult, and we’re here to help you in any way we can," reassures them that their feelings are normal and accepted.
- Example 3: Handling Emotional Outbursts
- A senior might have an emotional outburst due to frustration or fear, perhaps lashing out verbally. Instead of reacting defensively or critically, a non-judgmental approach would involve recognizing that the outburst is a result of underlying emotions, not a personal attack. Responding calmly and with understanding, such as, "I can see you’re upset, and I’m here to help you through this," helps de-escalate the situation and shows the senior that their feelings are respected.
- Example 4: Supporting Difficult Decisions
- A senior might make a decision that seems risky or unwise from a caregiver’s perspective, such as refusing certain medical treatments. A non-judgmental response would involve exploring their reasons without imposing your own views. For example, saying, "I respect your decision, and I’m here to support you. Can we talk about any concerns you have and how we can ensure you feel comfortable with your choices?" This approach respects the senior’s autonomy and fosters an open, supportive dialogue.
In the journey of caring for seniors, the roles of active
listening and empathy cannot be overstated. These essential skills transform
everyday interactions into meaningful connections, where seniors feel truly
seen, heard, and valued. By offering our full attention, reflecting on what is
communicated, asking open-ended questions, and responding with compassion, we
not only gather important information about the senior’s needs but also affirm
their dignity and worth.
Empathy goes beyond merely understanding another's
situation; it involves feeling with them and offering genuine, non-judgmental
support. Whether through emotional awareness, perspective-taking, or
compassionate responses, empathy allows us to bridge the gap between us and
those we care for, fostering trust and deepening relationships.
As healthcare and community care providers, our goal should
be to create a safe, respectful space where seniors can express themselves
freely, knowing they will be met with kindness and understanding. By
integrating active listening and empathy into our daily practices, we not only
improve the quality of care but also enrich the lives of those we serve.



.jpg)










Comments
Post a Comment