The Silent Epidemic: Understanding Fatty Liver Disease
Understanding Fatty Liver Disease
Fatty liver disease occurs when excess fat accumulates in
liver cells, leading to inflammation and damage. Fatty liver disease is
broadly categorized into two main types:
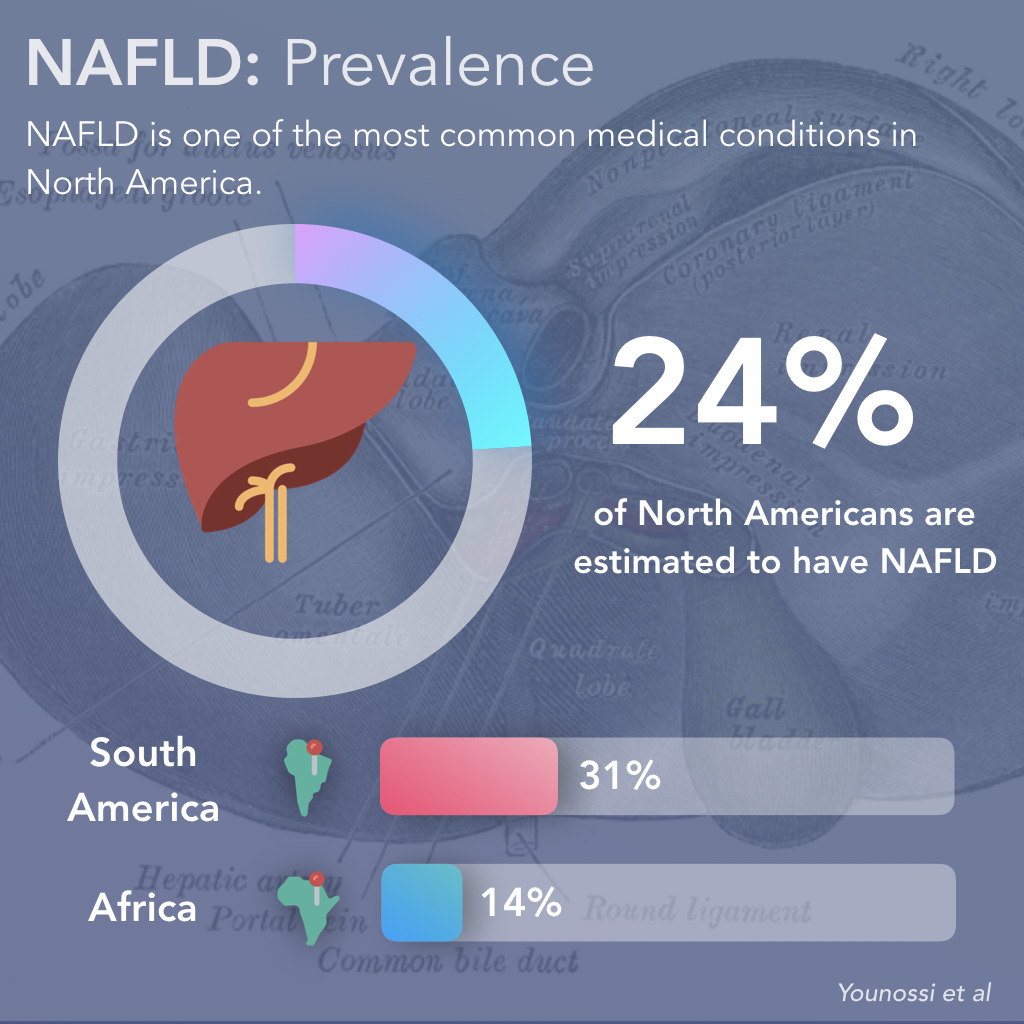
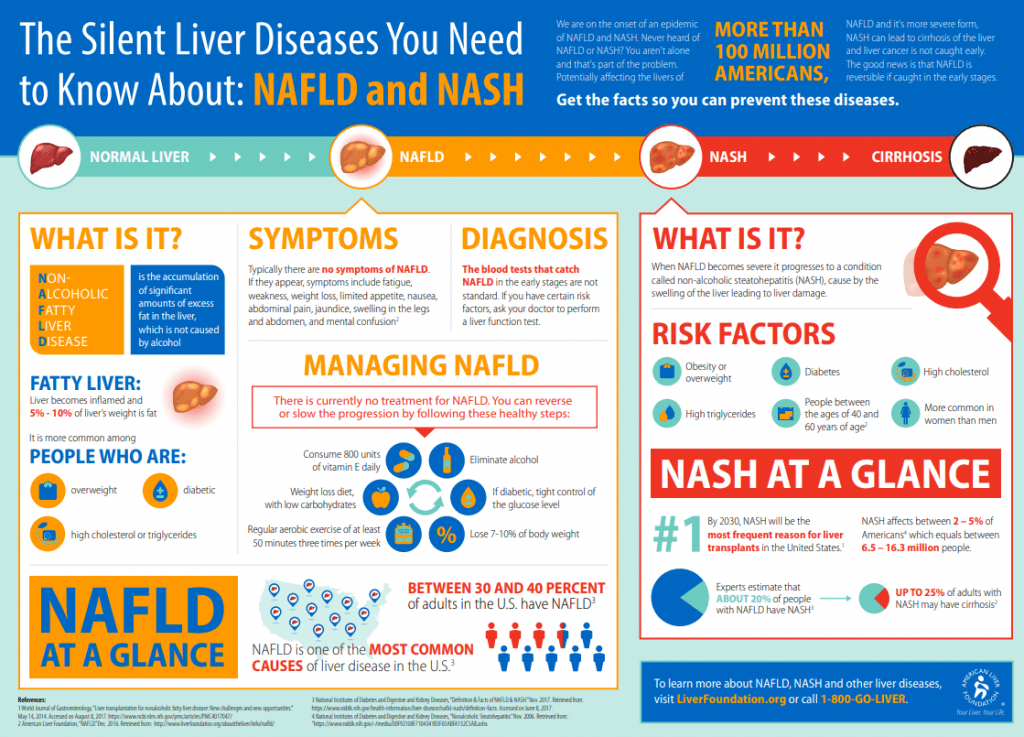
Non-alcoholic fatty liver disease (NAFLD): This is
the most common type, affecting individuals who don't consume excessive amounts
of alcohol. It's strongly associated
with metabolic syndrome, a cluster of conditions including obesity, insulin
resistance, high blood pressure, high triglycerides, and high blood sugar. The
exact mechanisms driving NAFLD are still being researched, but the accumulation
of fat in the liver is believed to be triggered by a combination of factors:
- Insulin
Resistance: This is a central feature of NAFLD. When the body
becomes resistant to insulin, it leads to increased levels of fat in the
blood, which are then deposited in the liver. This insulin resistance also
leads to increased production of fat within the liver itself.
- Increased
Fat Production: The liver produces more fat than it can
metabolize, leading to an accumulation of fat droplets within the liver
cells.
- Decreased
Fat Breakdown: The liver's ability to break down fat is impaired,
contributing to the buildup of fat.
- Inflammation: In
many cases, NAFLD progresses to non-alcoholic steatohepatitis (NASH),
which involves inflammation and damage to liver cells. This inflammation
can lead to scarring (fibrosis) and ultimately cirrhosis, a severe and
irreversible stage of liver damage.
- Genetic Factors: Genetic predisposition plays a role in the development of NAFLD, with certain genes increasing the risk.
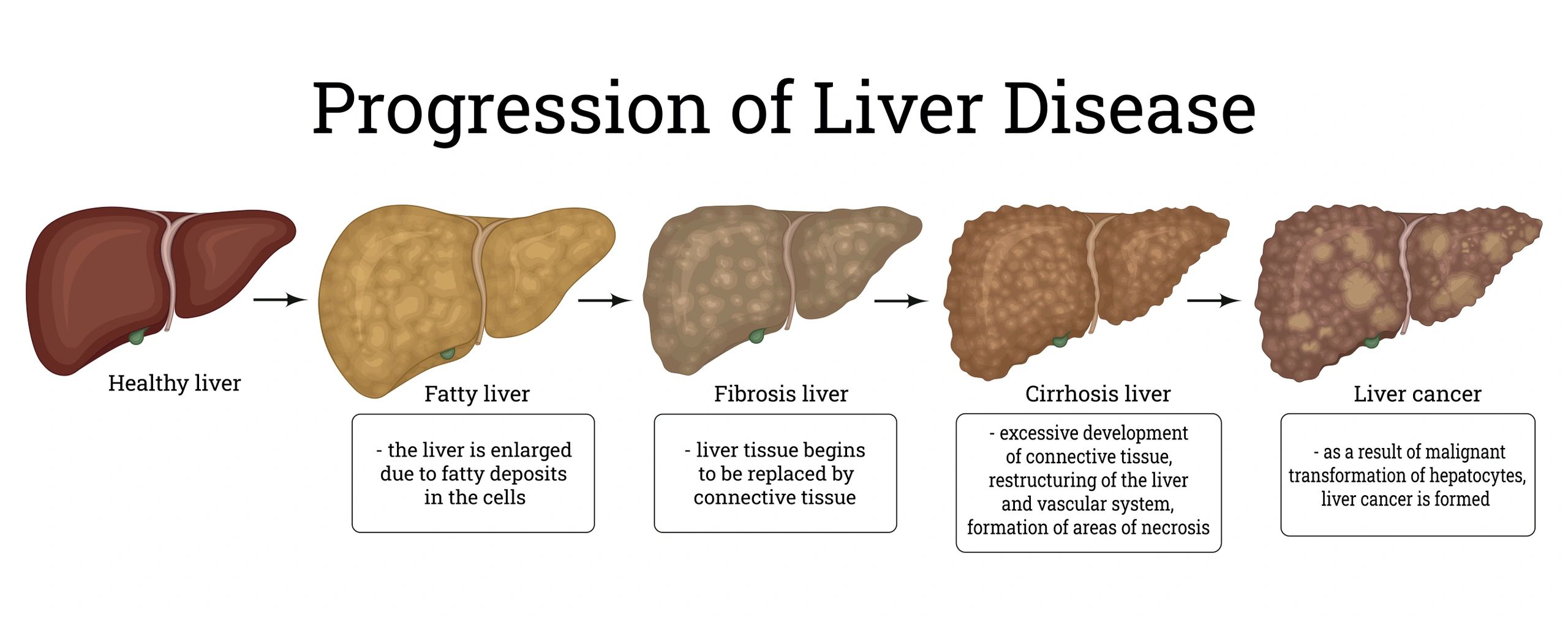
NAFLD progresses through several stages:
- Simple fatty liver: Excess fat accumulates in the liver without causing significant inflammation or damage.
- Non-alcoholic steatohepatitis (NASH): Inflammation and cell damage occur in the liver, potentially leading to scarring.
- Fibrosis: Scar tissue develops in the liver, impairing its function.
- Cirrhosis: Severe scarring leads to significant liver damage, potentially resulting in liver failure, liver cancer, or the need for a liver transplant.
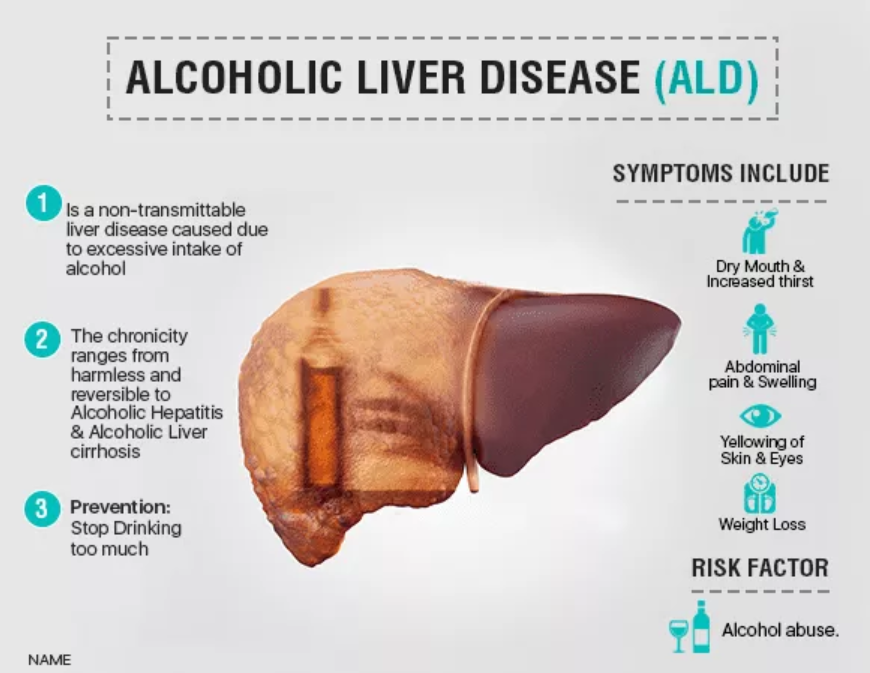
Alcoholic fatty liver disease (AFLD): This type is caused by excessive alcohol consumption. Alcohol is metabolized primarily in the liver, and the process of metabolizing alcohol can directly damage liver cells and lead to fat accumulation.
The severity of AFLD depends on the amount and duration of alcohol consumption.
- Direct
Liver Cell Damage: Alcohol directly damages liver cells, causing
inflammation and impairing their function. This damage can lead to fat
accumulation and the development of steatosis.
- Increased
Fat Production: Alcohol consumption can increase the liver's
production of fat, further contributing to fat accumulation.
- Decreased
Fat Breakdown: Similar to NAFLD, alcohol can impair the liver's
ability to break down fat, leading to a buildup of fat droplets in liver
cells.
- Inflammation: Alcohol consumption causes inflammation in the liver, leading to steatohepatitis (alcoholic steatohepatitis or ASH). This inflammation can progress to fibrosis and cirrhosis.
The more alcohol that you drink, the more you damage your liver. Alcoholic fatty liver disease is the earliest stage of alcohol-related liver disease. The next stages are alcoholic hepatitis and cirrhosis. Alcoholic fatty liver disease only happens in people who are heavy drinkers, especially those who have been drinking for a long period of time. The risk is higher for heavy drinkers who are women, have obesity, or have certain genetic mutations.
While both NAFLD and AFLD lead to fat accumulation in the
liver, their underlying causes and mechanisms differ significantly. NAFLD is
strongly linked to metabolic syndrome and obesity, while AFLD is directly
caused by excessive alcohol consumption. Both conditions can progress to
serious complications, emphasizing the importance of early detection, lifestyle
modifications, and appropriate medical management.
Causes of Fatty Liver Disease
Fatty liver disease, characterized by the buildup of excess
fat in the liver, can arise from various factors. Let's explore the major
causes in detail:
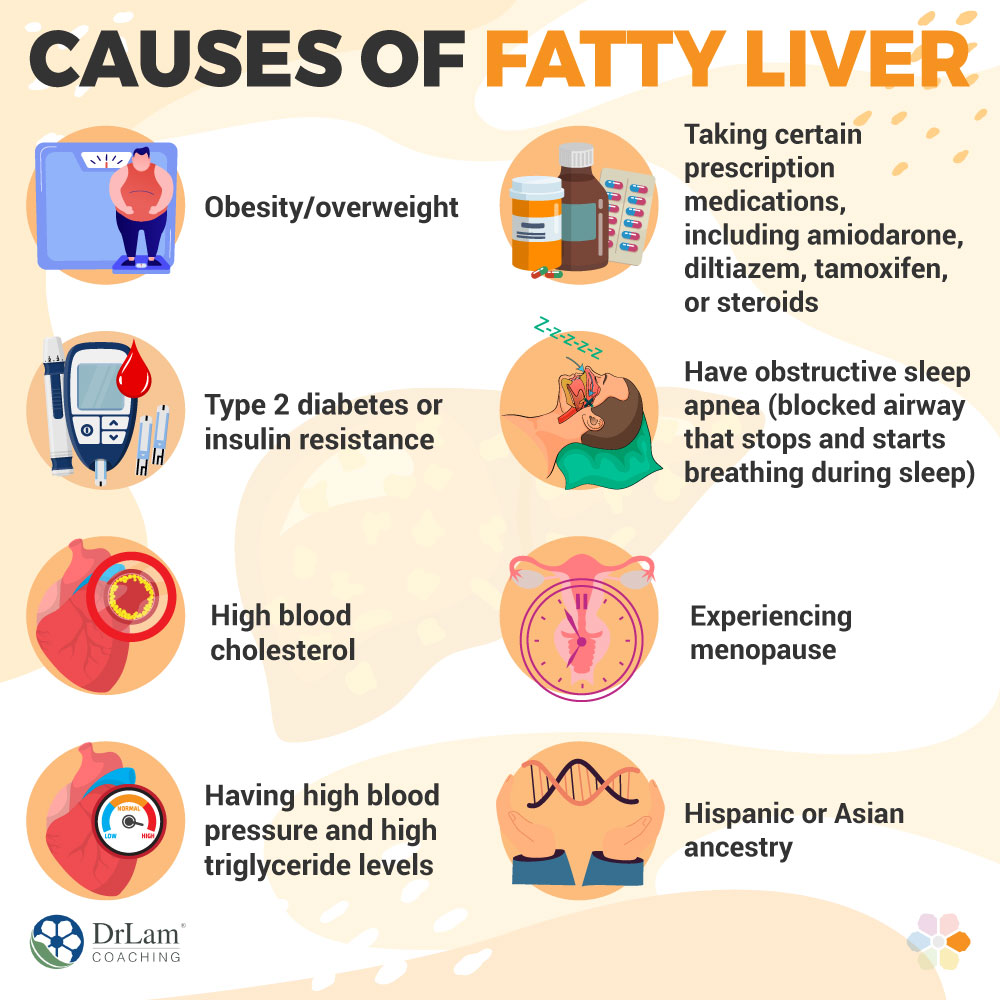
Obesity is the most significant risk factor for
non-alcoholic fatty liver disease (NAFLD). When individuals are overweight or
obese, their bodies store excess fat in various locations, including the liver.
This excess fat accumulation disrupts the liver's normal functioning, leading
to inflammation and potential damage.
- Mechanism: Obesity
triggers a complex interplay of metabolic changes. Excess fat cells
release inflammatory substances, contributing to liver inflammation.
Furthermore, obesity is often associated with insulin resistance, a
condition where the body doesn't respond effectively to insulin, leading
to increased blood sugar and fat storage in the liver. This vicious cycle
exacerbates fat accumulation and liver damage.
Insulin resistance is a key player in the development of
NAFLD. Insulin, a hormone produced by the pancreas, helps regulate blood sugar
levels. When the body becomes resistant to insulin, it struggles to use glucose
(sugar) for energy, leading to increased blood sugar levels and fat
accumulation in the liver.
- Mechanism: Insulin
resistance disrupts the liver's ability to process and break down fats.
This leads to an accumulation of fat droplets within liver cells,
contributing to the development of steatosis (fatty liver). Furthermore,
insulin resistance promotes inflammation, potentially progressing to
non-alcoholic steatohepatitis (NASH), a more severe form of NAFLD.
3. High Triglycerides
Triglycerides are a type of fat found in the blood. High
levels of triglycerides are another significant risk factor for NAFLD. Excess
triglycerides can be deposited in the liver, contributing to fat accumulation
and inflammation.
- Mechanism: Elevated
triglycerides can impair the liver's ability to process and break down
fats efficiently. This leads to a buildup of fat within liver cells,
potentially progressing to NASH. High triglycerides are often associated
with other metabolic disorders, such as obesity, insulin resistance, and
metabolic syndrome, further increasing the risk of NAFLD.
Genetics plays a role in the susceptibility to developing
NAFLD. Some individuals have a genetic predisposition that makes them more
likely to develop the condition, even if they don't have other risk factors
like obesity or insulin resistance.
- Mechanism: Specific
genes influence the liver's metabolism of fats, its sensitivity to
insulin, and its susceptibility to inflammation. Variations in these genes
can increase the risk of developing NAFLD and its progression to more
severe stages.
Some medications can contribute to fat accumulation in the
liver. These medications include:
- Steroids: Long-term
use of steroids can lead to fat accumulation in the liver.
- Anti-seizure
medications: Certain anti-seizure medications can also contribute to
fatty liver.
- Chemotherapy
drugs: Some chemotherapy drugs can cause liver damage and fat
accumulation.
- Mechanism: The
exact mechanisms by which these medications contribute to NAFLD vary, but
they often involve disrupting the liver's metabolism of fats or increasing
inflammation.
Excessive alcohol consumption is the primary cause of
alcoholic fatty liver disease (AFLD). Alcohol is metabolized primarily in the
liver, and the process of metabolizing alcohol can directly damage liver cells
and lead to fat accumulation.
- Mechanism: Alcohol
metabolism produces toxic byproducts that can damage liver cells, leading
to inflammation and impaired function. This damage can lead to fat
accumulation and the development of steatosis. Furthermore, alcohol
consumption can increase the liver's production of fat, further
contributing to fat buildup. Excessive alcohol consumption can also impair
the liver's ability to break down fat, leading to a buildup of fat
droplets in liver cells.
7. Rapid Weight Loss
Rapid weight loss, especially through extreme dieting or
bariatric surgery, can sometimes contribute to NAFLD. This is because the body
may not be able to adjust quickly enough to the sudden changes in fat
metabolism, leading to fat accumulation in the liver.
- Mechanism: Rapid
weight loss can disrupt the body's hormonal balance, affecting the liver's
ability to process and break down fats. This can lead to a temporary
buildup of fat in the liver, which may resolve over time as the body
adapts to the new weight.
Chronic malnutrition, especially protein deficiency, can
also contribute to NAFLD. Protein is essential for liver function, and a lack
of protein can impair the liver's ability to process fats.
- Mechanism: Protein
deficiency can lead to a buildup of fat in the liver, as the liver
struggles to break down and metabolize fats efficiently. Additionally,
malnutrition can weaken the immune system, making the liver more
susceptible to inflammation and damage.
- Metabolic
Syndrome: This cluster of conditions, including obesity, high blood
pressure, high triglycerides, and insulin resistance, significantly
increases the risk of NAFLD.
- Polycystic
Ovary Syndrome (PCOS): PCOS is a hormonal disorder that can increase
the risk of NAFLD.
- Sleep
Apnea: Obstructive sleep apnea, a condition where breathing
repeatedly stops and starts during sleep, is associated with an increased
risk of NAFLD.
- Certain
Infections: Some infections, such as hepatitis C, can contribute to
NAFLD.
Symptoms of Fatty Liver Disease
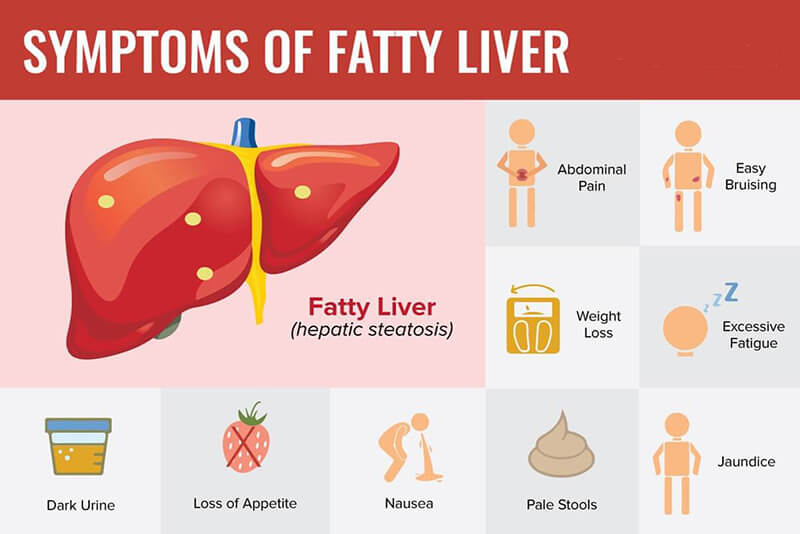
In its early stages, NAFLD often has no noticeable symptoms. As the disease progresses, symptoms may include:
- Fatigue. Fatty liver disease can cause fatigue, weakness, and a general feeling of being unwell.
- Abdominal pain or discomfort. As the liver becomes inflamed, you may experience abdominal swelling and pain.
- Loss of appetite. As the liver becomes damaged, you may experience weight loss, nausea, and vomiting.
- Jaundice. In severe cases, fatty liver disease can cause jaundice, a yellowing of the skin and eyes.
- Swelling in the legs or ankles.
The absence of early symptoms highlights the importance of
regular checkups and proactive health management, especially for individuals at
risk.
Diagnosis of Fatty Liver Disease
Diagnosing fatty liver disease can be tricky because it
often doesn't cause noticeable symptoms in its early stages. However, it's
crucial to detect it early to prevent potential complications. Here's a
breakdown of the diagnostic process:
1. Medical History and Physical Exam
- Medical
History: Your doctor will ask detailed questions about your health,
including:
- Alcohol
Consumption: They'll inquire about your alcohol intake to
differentiate between NAFLD (non-alcoholic fatty liver disease) and AFLD
(alcoholic fatty liver disease).
- Medications: They'll
ask about any medications you're taking, as some can contribute to fatty
liver.
- Family
History: They'll inquire about any family history of liver disease,
as genetic predisposition can play a role.
- Lifestyle
Factors: They'll ask about your diet, exercise habits, and overall
lifestyle, as these factors are strongly linked to NAFLD.
- Physical
Exam: Your doctor will perform a physical exam to check for signs of
liver enlargement, jaundice (yellowing of the skin and eyes), or other
signs of liver damage. They may also check your weight and height to
calculate your body mass index (BMI).
- Liver
Enzyme Tests: Blood tests are crucial to assess liver function.
Elevated levels of liver enzymes, such as alanine aminotransferase (ALT)
and aspartate aminotransferase (AST), can indicate liver damage.
- Other
Blood Tests: Your doctor may order additional blood tests to check
for:
- Blood
Sugar: To assess for insulin resistance and diabetes.
- Lipid
Profile: To measure cholesterol and triglyceride levels, which are
linked to NAFLD.
- Complete
Blood Count: To assess overall health and rule out other conditions.
- Ultrasound: An
abdominal ultrasound is often the first imaging test used to diagnose
fatty liver. It can visualize the liver and identify fat accumulation.
- Computed
Tomography (CT) Scan: CT scans can provide more detailed images of
the liver and help assess the extent of fat accumulation.
- Magnetic
Resonance Imaging (MRI): MRI can provide even more detailed images of
the liver and can be used to assess for inflammation and scarring.
- Elastography: This
newer imaging technique measures the stiffness of the liver, which can
indicate the presence of fibrosis (scarring). There are different types of
elastography, including:
- Transient
Elastography: Uses ultrasound waves to measure liver stiffness.
- Magnetic
Resonance Elastography: Combines MRI with sound waves to create a
visual map of liver stiffness.
- Purpose: A
liver biopsy is the gold standard for diagnosing NASH (non-alcoholic
steatohepatitis) and assessing the severity of liver damage. It involves
taking a small sample of liver tissue for microscopic examination.
- When
It's Needed: A liver biopsy is usually recommended when:
- Other
tests suggest advanced liver disease or NASH.
- Test
results are unclear.
- To
rule out other liver diseases.
Interpreting Results:
- NAFLD: If
the tests reveal fat accumulation in the liver but no significant
inflammation or scarring, the diagnosis is NAFLD.
- NASH: If
the tests show both fat accumulation and inflammation, along with evidence
of fibrosis, the diagnosis is NASH.
- AFLD: If
the tests indicate significant alcohol consumption and liver damage, the
diagnosis is AFLD.
- Early
Detection: Early diagnosis is crucial for preventing complications.
If you have risk factors for fatty liver disease, talk to your doctor
about getting screened.
- Lifestyle
Modifications: Lifestyle changes, such as weight loss, a healthy
diet, and regular exercise, are essential for managing NAFLD.
- Treatment: Treatment
for fatty liver disease depends on the type and severity of the condition.
Your doctor will recommend the most appropriate treatment plan for you.
Treatment and Management of Fatty Liver Disease
Currently, there's no specific medication to cure NAFLD. The
focus is on managing the condition and preventing its progression through
lifestyle modifications:
Weight loss: Even modest weight loss can
significantly improve liver health. Bariatric surgery-induced weight loss has
shown positive effects on lipid profiles, hepatic steatosis, steatohepatitis,
and long-term mortality. While promising, bariatric surgery is not considered a
primary treatment for NASH, but rather a potential option for morbidly obese
patients with significant liver disease.
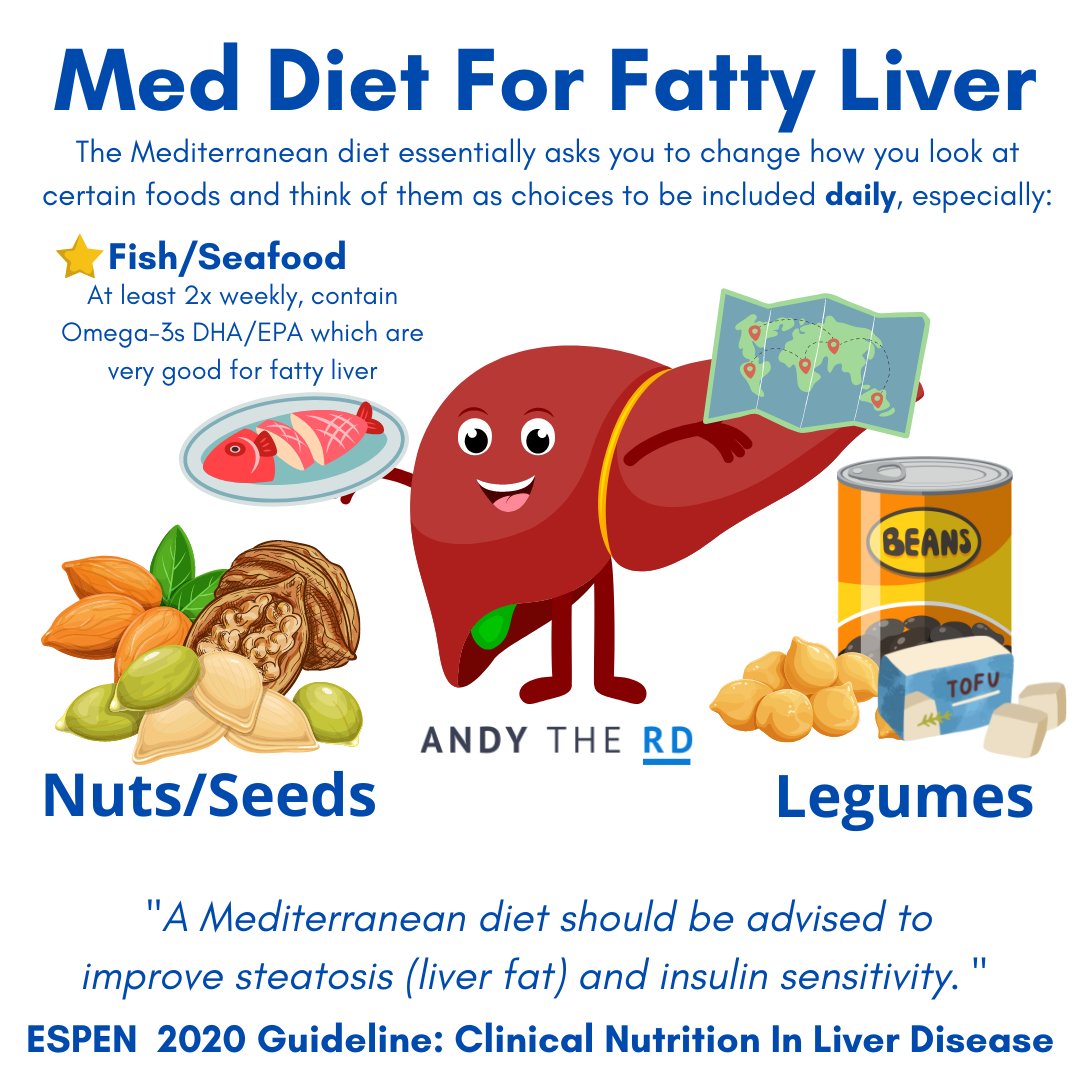
Healthy diet: A balanced diet low in saturated and
trans fats, cholesterol, and added sugars is crucial. Focus on fruits,
vegetables, whole grains, and lean proteins. The Mediterranean diet, rich in
fruits, vegetables, whole grains, and healthy fats, has shown promise in
improving liver health, insulin sensitivity, and reducing cardiovascular risk.
Regular exercise: Regular physical activity improves insulin sensitivity and helps reduce fat storage. Includes both aerobic and strength training is crucial for weight management, insulin sensitivity, and reducing inflammation that can contribute to better liver health.
Alcohol avoidance: Completely avoiding alcohol is
essential, particularly for individuals with AFLD.
Medication: Medications may be prescribed to manage
related conditions such as diabetes or high cholesterol. While not a cure, vitamin E has shown some
benefit in non-diabetic patients with biopsy-proven NASH (non-alcoholic
steatohepatitis). However, long-term safety and efficacy are still under
investigation. The insulin sensitizer pioglitazone, typically used for type 2
diabetes, may improve liver function in non-diabetic patients with NASH, but
long-term safety and efficacy are not fully established. Further, cenicriviroc is being investigated
for its potential to reduce inflammation and fibrosis in NASH.
Regular monitoring and follow-up with a healthcare provider
are crucial for managing NAFLD and preventing complications.
Preventing Fatty Liver Disease
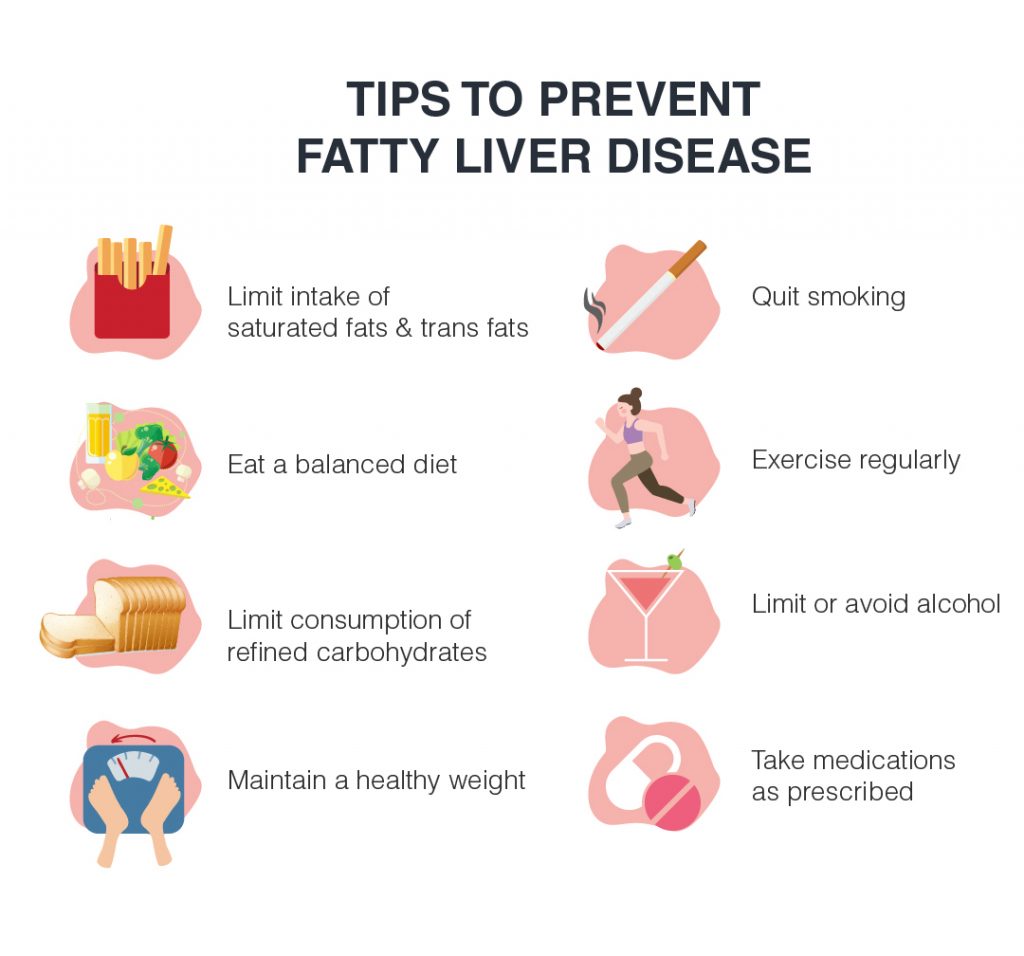
Preventing fatty liver disease is all about adopting a healthy lifestyle that minimizes the risk factors associated with this condition.
1. Maintain a Healthy Weight:
- Excess
Weight: Obesity is a major risk factor for NAFLD (non-alcoholic
fatty liver disease). Excess weight, especially around the abdomen
(visceral fat), puts a strain on the liver and promotes fat accumulation.
- Weight
Loss: Losing even a small amount of weight (5-10% of your body
weight) can significantly improve liver health and reduce fat buildup.
- Sustainable
Strategies: Focus on sustainable weight loss strategies that
include a balanced diet and regular exercise. Avoid crash diets or extreme
measures that can be harmful in the long run.
- Limit
Sugary Foods and Drinks: Added sugars, especially fructose, can
contribute to fat accumulation in the liver. Reduce your intake of sugary
drinks, processed foods, and desserts.
- Choose
Whole Foods: Focus on a diet rich in fruits, vegetables, whole
grains, and lean protein sources. These foods provide essential nutrients
and fiber, which can help regulate blood sugar levels and promote healthy
digestion.
- Healthy
Fats: Include healthy fats in your diet, such as those found in
olive oil, avocados, nuts, and fatty fish. These fats can help reduce
inflammation and improve liver function.
- Limit
Saturated and Trans Fats: These unhealthy fats can increase
cholesterol levels and contribute to fat buildup in the liver. Avoid red
meat, processed foods, and fried foods high in saturated and trans fats.
- Benefits
of Exercise: Regular physical activity can help you lose weight,
improve insulin sensitivity, and reduce inflammation. All of these factors
contribute to better liver health.
- Moderate-Intensity
Exercise: Aim for at least 150 minutes of moderate-intensity
aerobic activity or 75 minutes of vigorous-intensity aerobic activity per
week.
- Strength
Training: Incorporate strength training exercises at least twice
a week to build muscle mass and improve metabolism.
- Excessive
Alcohol: Heavy alcohol consumption is a major cause of alcoholic
fatty liver disease (AFLD). Even moderate alcohol intake can increase the
risk of NAFLD.
- Moderation: If
you choose to drink alcohol, do so in moderation. For women, that means no
more than one drink per day, and for men, no more than two drinks per day.
- Abstaining: If
you have fatty liver disease, it's best to abstain from alcohol entirely.
- Diabetes: People
with type 2 diabetes are at increased risk of NAFLD. Managing blood sugar
levels through medication and lifestyle changes is essential for
preventing liver damage.
- High
Blood Pressure and Cholesterol: These conditions can contribute
to NAFLD. Working with your doctor to manage blood pressure and
cholesterol levels is important.
- Metabolic
Syndrome: Metabolic syndrome is a cluster of conditions that
increase the risk of heart disease, stroke, and type 2 diabetes. It also
increases the risk of NAFLD. Managing these conditions can help protect
your liver.
- Early
Detection: Early detection of fatty liver disease is crucial for
preventing complications. If you have risk factors for NAFLD, talk to your
doctor about getting screened.
- Liver
Function Tests: Regular blood tests can assess liver function and
identify any signs of damage.
- Smoking
and Liver Health: Smoking can damage the liver and increase the
risk of liver cancer. Quitting smoking is one of the best things you can
do for your liver health.
- Milk
Thistle: Milk thistle is a natural herb that may help protect the
liver from damage. However, more research is needed to confirm its
effectiveness.
- Vitamin
E: Some studies suggest that vitamin E supplements may be
beneficial for people with NAFLD. Talk to your doctor before taking any
supplements.
Preventing fatty liver disease is a proactive approach to maintaining overall health. By adopting a healthy lifestyle, managing underlying medical conditions, and getting regular checkups, you can significantly reduce your risk of developing this condition. Always consult with your doctor for personalized advice and guidance.




Comments
Post a Comment